Some of the challenges of being an optometrist today include public and private reimbursement issues and adopting emerging technologies such as tele-optometry and AI into practice.
As an optometrist practising in Ontario that means billing OHIP for your time (for provincially covered services). For services not covered by OHIP (like tele-optometry), they can be billed directly to the patient.
Therefore, it’s important to know the ins and outs of OHIP billing so you are paid for the work you do. However, you cannot bill OHIP for any of the time you spend on reviewing patient files and admin work, including billing.
That’s why accurate billing is essential. Unfortunately, billing errors are common and end up with claim rejections that waste time and delay payments. To help save you time, we’ve put together an optometry OHIP billing code guide.
Along with this Guide, keep the Ontario Schedule of Benefits Optometry Services handy. It provides ministry guidelines, fee codes for billing purposes and dollar amounts that correspond to each service you provide.
Major Eye Examination Codes
-
V404 Major oculo-visual examination for patients age 19 years or less
-
V406 Major oculo-visual examination for patients age 65 years or older with no eligible medical conditions
-
V407 Major oculo-visual examination for patients age 65 years or older with one or more eligible medical conditions*
-
V409 Major oculo-visual examination for patients age 20 to 64 years with one or more eligible medical conditions*
Requirements: valid requisition from a physician or a registered nurse.
Eligible medical conditions: Diabetes Mellitus, Glaucoma, Cataract, Retinal Disease, Amblyopia, Visual Field Defects, Corneal Disease, Strabismus, Recurrent Uveitis and Optic Pathway Disease.
Major Eye Examination includes:
- Relevant history
- Visual acuity examination
- Ocular motility examination
- Refraction and written refractive prescription if required
- Slit lamp examination of the anterior segment
- Ophthalmoscopy by one or more direct binocular indirect ophthalmoscope, monocular indirect ophthalmoscope or no contact fundus lens
- Advice /instruction to the patient
- Letter outlining the findings of examination
- Tonometry
- Visual field examination by confrontation field
- Dilated fundus examination by one or more direct binocular indirect ophthalmoscope, monocular indirect ophthalmoscope or no contact fundus lens
Minor Eye Examination Codes
- V402 Oculo-visual minor assessment for patients age 19 years or less or patients age 19 years or less or age 64 years or more
- V408 Oculo-visual minor assessment for patients age 20 to 64 years
- Assessment of the eye and vision system clinically required for the purpose of assessing or reassessing a single ocular condition
- History or presenting complaint
- Advice/instruction to the patientV415 Oculo-visual minor assessment for patients age 65 years or older
Note: V409 must have been rendered within a 12-month period preceding the date of the oculo-visual minor assessment.
Automated Visual Fields Assessment
V410 Assessment of the eye and vision system for the purpose of mapping patient’s visual fields
- Patients age 19 years or less or 64 years or older, the service is insured when the automated visual field assessment is clinically necessary to determine the extent and sensitivity or the patient’s visual fields
- Patients age 20-64 years, the service in insured when following a major eye examination (V409) or a minor assessment (V408)
MSCC Ontario Disability Support Program (ODSP)
V450 Periodic oculo-visual assessment rendered to patients age 20-64 years who are recipients of income support under the Ontario Disability Support Program Act
MCSS Ontario Works Program (OW)
V451 Periodic oculo-visual assessment rendered to patients age 20-64 years who are recipients of income assistance or benefits under the Ontario Works Act
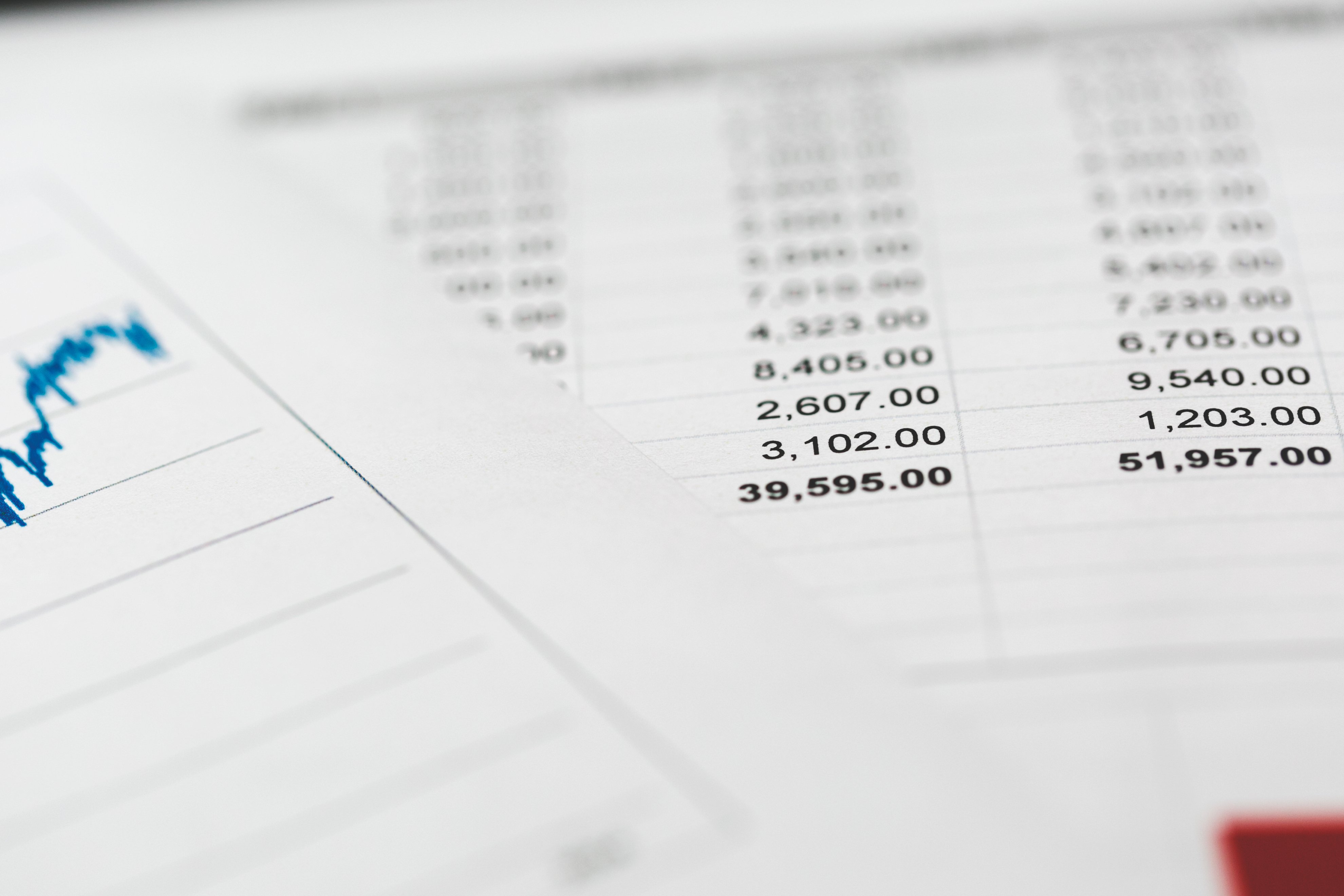
Optometry OHIP Diagnostic Codes
| Diagnostic | Code |
|---|---|
| Aphakia | 360 |
| Retinal Detachment | 361 |
| Hypertensive Retinopathy | 362 |
| Chorioretinitis | 363 |
| Iritis | 364 |
| Glaucoma | 365 |
| Cataract, excludes diabetic or congenital | 366 |
| Myophia astigmatism | 367 |
| Amblyopia, Visual field defects | 368 |
| Blindness and low vision | 369 |
| Keratitis, corneal ulcer | 370 |
| High Myopia greater than 9 diopters | 371 |
| Conjunctiva disorders | 372 |
| Blepharitis, chalazion, style | 373 |
| Other eyelid disorders | 374 |
| Dacryocystitis, obstruction of lacrimal duct | 375 |
| Keratoconus | 376 |
| Optic neuritis | 377 |
| Strabismus | 378 |
| Other disorders of the eye | 379 |
Optometry OHIP Billing Tips to Avoid Submission Errors
If you receive a submission error then your claim did not pass OHIP’s pre-edit approval process. While this will delay your payment, submission errors are usually simple to correct. In fact, the most common submission errors are a direct result of the following:
- A fee code conflict – for example, your diagnostic code doesn’t match with your billing code
- Invalid insurance coverage – your patient does not have a valid OHIP card
- Admission dates – admission dates should not be added to patient profiles or claims; they are only needed when seeing hospital in-patients
Always check those three things before submitting a claim to OHIP. If you do get a submission error it will be outlined in your Claim Error Report using a specific code. This code will explain what rule you violated.
How to Avoid Claim Rejections
Initial claims have to be submitted within three months of the original date of service. Any claim submitted after three months will be rejected and become ‘stale dated‘ claims.
Other common rejections in optometry OHIP billing are often caused by errors in follow-up visits. For example, if you see a patient who is covered under OHIP and they have a follow-up visit, that visit is only billable if it is claimed with the same diagnostic as in the original exam. If the follow-up is billed with a different diagnostic your claim will be rejected. Additionally, make sure the follow-up is billed on a different date of service than the full exam.
When a claim is rejected or a claim is reduced, you can resubmit the claim and inquire to appeal the decision. To inquire about your rejected claims you need to fill out the Remittance Advice Inquiry form. Claim resubmissions must be completed within four months from the issue date of the RA report.
Questions? Contact us if you have any questions regarding Optometry OHIP Billing Codes. We’d be happy to give you a walkthrough of how Dr.Bill helps hundreds of optometrists and optometry groups submit OHIP claims in seconds!
This article offers general information only and is not intended as legal, financial or other professional advice. A professional advisor should be consulted regarding your specific situation. While information presented is believed to be factual and current, its accuracy is not guaranteed and it should not be regarded as a complete analysis of the subjects discussed. All expressions of opinion reflect the judgment of the author(s) as of the date of publication and are subject to change. No endorsement of any third parties or their advice, opinions, information, products or services is expressly given or implied by RBC Ventures Inc. or its affiliates.