How to Bill COVID-19 Fee Codes K087A, K088A, K089A for Uninsured Patients
OHIP has released a clarification on how to bill fee codes K087A, K088A, and K089A (see code descriptions below).
When submitting claims for K087A and K088A, the fee value on the claim should equal the value of the fee code multiplied by the total number of patients served during the same day.
For example, if K087A is claimed for 3 patients seen during the same day, the fee billed should be $71.25 (3 x $23.75). K089A is time based and must be the total number of half hour units for all patients served during the same day.
How To Bill For Uninsured Patients on Dr.Bill
On Dr.Bill, when you bill K087, K088 and K089 you need to make sure you have the following information:
- Service date
- Service code
- Units: If the If you see more than one uninsured patient on the same day for the same service code, they all need to be billed on one claim and represented in units. (For example, if you see 3 patients in one day for a K087A, instead of 3 individual claims, you will bill one claim for 3 units of K087A. Otherwise, only 1 claim will be paid and the rest will kick back as duplicate billing. If you’re billing K089 (the counselling code for psychiatrists), 1 unit = every 30 minutes spent with a patient.
- Note Section: Add the names of each patient
- Do not mark these claims for manual review or they will not be processed for payment
Note that Dr.Bill will have the “dummy/anonymous” patient profile ready for you. You do not have to create your own.
Fee Codes and Payment
K087: minor assessment of an uninsured patient provided in-person or by telephone or video or advice or information provided in-person or by telephone or video to an uninsured patient’s representative regarding health maintenance, diagnosis, treatment and/or prognosis-$23.75.
K088:
- intermediate assessment of an uninsured patient provided in-person or by telephone or video, or advice or information provided in-person or by telephone or video to an uninsured patient’s representative regarding health maintenance, diagnosis, treatment and/or prognosis, if the service lasts a minimum of 10 minutes; or
- psychotherapy, psychiatric or primary mental health care, counselling or interview conducted by telephone or video, if the service lasts a minimum of 10 minutes-$36.85
K089: psychotherapy, psychiatric or primary mental health care, counselling or interview conducted in-person or by telephone or video per unit (unit means half hour or major part thereof)-per unit $67.75.
Claim submissions for these codes must also adhere to the following requirements:
- The claim must be submitted with the Billing Number of the physician who provided the service.
- The Health Number field on the claim must be left blank. If a physician submits these claims with a Health Number (HN), the claim will reject ‘VHB-No HN Required for FSC’.
- The Version Code field on the claim must be left blank. If a physician submits these claims with a Version Code, the claim will reject ‘VHB-No HN Required for FSC’.
- The Birth Date field on the claim must be left blank. If a physician submits these claims with a value in the Birth Date, the claim will reject ‘VH1-Invalid Health Number’.
- The Service Date on the claim will be the date the service was provided.
- The claim must be submitted with a fee billed value not equal to $0.00. If a physician submits these claims with a fee billed value of $0.00, the claim will pay $0.00.
If, at any time, you have any questions don’t hesitate to get in touch. Otherwise, please check back to the COVID-19 Resource centre for more updates.
This article offers general information only and is not intended as legal, financial or other professional advice. A professional advisor should be consulted regarding your specific situation. While information presented is believed to be factual and current, its accuracy is not guaranteed and it should not be regarded as a complete analysis of the subjects discussed. All expressions of opinion reflect the judgment of the author(s) as of the date of publication and are subject to change. No endorsement of any third parties or their advice, opinions, information, products or services is expressly given or implied by RBC Ventures Inc. or its affiliates.
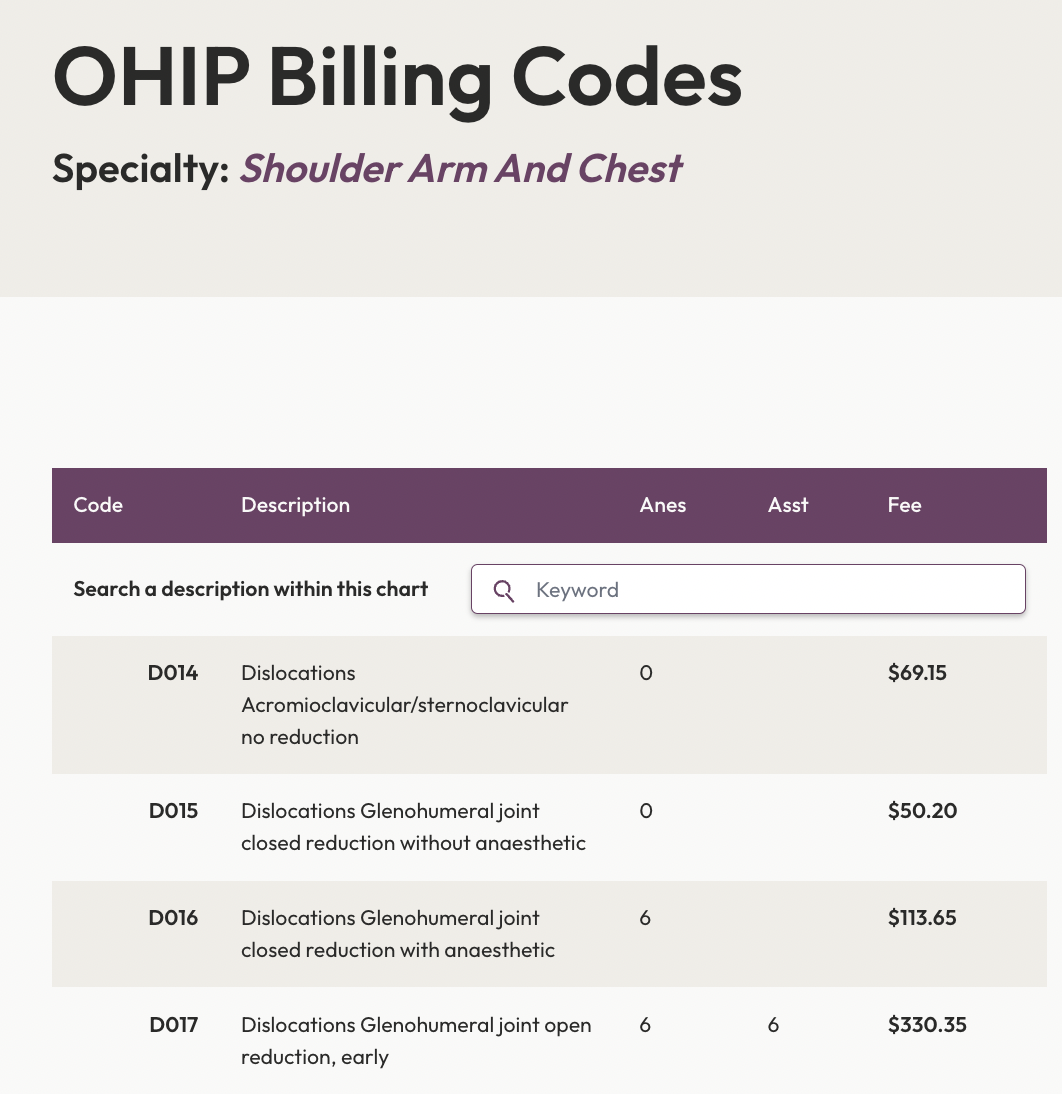
Search All OHIP Billing Codes
Search the Ontario Schedule of Medical Benefits electronically. We’ve digitized all the OHIP billing codes so you can easily find the most up to date billing rules and amounts.