If you are practicing Family and General Medicine in Ontario knowing which fee codes to use can quickly get confusing. The complexity of submitting claims to OHIP, on top of your already heavy workload, is bound to cause a few headaches.
To help save you time, we’ve put together a list of all the available fee codes and when/how to use them. Knowing which codes are available in your speciality is essential in order to make sure you’re getting properly paid for everything you do.
To review our complete list visit our searchable database of all OHIP Billing Codes.
Consultations & Assessments
You can give consultations and assessments in a number of environments such as private offices, walk in clinics, and hospitals for both inpatients and outpatients. Knowing the right code, and how often you can use it, can be the key to maximizing your billing and reducing refusals.
An assessment is the evaluation of a patient in a location other than their home. It requires taking a full history of the patient (to include the patient’s complaint, their medical history, past past medical history, social history, and a functional inquiry into all body parts and systems), as well as a physician examination or detailed examination of one or more parts/systems.
A consultation is an assessment but when there's a written request asking you to see a patient - either from a referring physician or a nurse practitioner who needs your opinion.
Consultations
You can only claim a consultation when it’s been specifically requested by the attending practitioner or NP - this means that on every consultation claim you need to name the referring physician.
Consultation Guidelines
You are only allowed to give one consultation service to the same patient for the same diagnosis per two consecutive 12 month periods except:
- When the additional consultation service is a repeat consultation as you’re allowed to see the patient for follow-up care provided by another physician in between visits.
- When you’ve given a consultation to a patient in any location before but you’ve been asked a second time to see the patient for the same condition. If this is the case then you’ll be able to give a total of two services per two consecutive 12 month periods only if:
However, if you see a patient for the second time within 12 months but for a completely unrelated diagnosis then you can bill for it. Consultations are limited to one every 12 months for the same diagnosis.
GP Consultation Fee Codes
- A005 Consultation
- A911 Special family and general practice consultation
- You must spend a minimum of 50 minutes with the patient (exclusive of the time spent providing any other separately billable services).
- A912 Comprehensive family and general practice consultation
- You must spend a minimum of 75 minutes with the patient (exclusive of the time spent providing any other separately billable services).
- A945 Special palliative care consultation
- You can bill this when you spend a minimum of 50 minutes with the patient and/or patient's representative/family. However the majority of time must be spent in consultation with the patient.
Repeat Consultation
- The second consultation is at a hospital inpatient or a patient in an Emergency Department.
- The second consultation happens more than 12 months but less than 24 months following the first consultation.
- A006 Repeat consultation
- A repeat consultation is an additional consultation given when your patient has the same problem as they had during the first consultation but after they’ve already received care from another physician.
Limited Consultation
- A905 Limited consultation
- A limited consultation is a consultation which is less demanding and, in terms of time, normally requires substantially less of your time than a full consultation. Otherwise, a limited consultation has the same requirements as a full consultation.
- H065: Consultation in Emergency Medicine
H105: In-patient interim admission orders
Telephone Consultations
- K734: Physician to physician telephone consultation _ Referring physician (Physician on duty in an emergency department or a hospital urgent care clinic)
- K735: Physician to physician telephone consultation _ Consultant physician (Physician on duty in an emergency department or a hospital urgent care clinic)
- K733: CritiCall telephone consultation _ Consultant physician
- K736: CritiCall telephone consultation _ Referring physician (Physician on duty in an emergency department or a hospital urgent care clinic)
- K737: CritiCall telephone consultation _ Consultant physician (Physician on duty in an emergency department or a hospital urgent care clinic)
- K739: Physician to physician e_consultation
Assessments
An assessment includes a detailed medical history aside from just the presenting issue and full physical exam. You’re allowed to give general assessments once every 12 months per patient. You may be eligible to claim more than 1 general assessment if:
- You see a patient for a second time for a complaint for which the diagnosis is clearly different and unrelated to the diagnosis made at the time of the first general assessment.
- At least 90 days have passed since the last general assessment and the second assessment is a hospital admission assessment.
- A003 General assessment
- A003 isn’t eligible if you see the patient at home. If it’s a home assessment bill A900 with special visit premiums (when the patient is elderly/frail/housebound).
- A004 General re-assessment
- A general re-assessment includes all the services listed for a general assessment, with the exception of the patient’s history, which you don’t need to include as all the details have already been obtained in the original assessment.
- With the exception of general re-assessments provided for hospital admissions (since a patient can be admitted an unlimited amount of times in a year, if needed), these are limited to two per 12 month period, per patient.
- A888 Emergency department equivalent (partial assessment)
- A partial assessment is the limited service that constitutes a history of the presenting complaint, the necessary physical examination, advice to the patient and appropriate record. It’s different from a full assessment in that a full assessment includes a detailed medical history aside from just the presenting issue and full physical exam.
- You can bill for A888 when you see a patient in the emergency department on a Saturday, Sunday or Holiday. It’s not eligible for any premiums. If it’s not on a weekend then bill a regular consult or assessment. A888 is specific to Emerg equivalents (i.e., an office or other place, including Urgent Care Centres, Walk-in Clinics, Extended Hours Clinics, or other settings other than a hospital emergency department) in which the only insured services provided are to patients who do not have pre-arranged appointments.
- A001 Minor assessment
- A minor assessment includes one or both of the following:
- A brief history and examination of the affected part or region (or related to a mental or emotional disorder).
- Your brief advice or information regarding the health maintenance, diagnosis, treatment and/or prognosis.
- A001 includes travelling to and from the home so Special Visit Premiums aren’t included.
- A minor assessment includes one or both of the following:
- A008 Mini assessment
- A mini assessment is when an assessment of a patient for an unrelated non-WSIB problem is provided during the same visit as an assessment of a WSIB related problem for which only a minor assessment was given.
- A007 Intermediate assessment or well baby care
- An intermediate assessment is a primary care GP service that requires a more extensive examination than a minor assessment but less medical history needed than a general assessment. It requires a history of the presenting complaint, inquiry concerning, and examination of the affected parts, regions, systems, or mental or emotional disorder as needed to make a diagnosis, exclude disease, and/or assess function.
- A007 includes travelling to and from the home so Special Visit Premiums aren’t included.
- A900 Complex house call assessment
- A complex house call assessment is for any primary care service that you give in a patient’s home. The patient must be considered either a frail elderly patient or a housebound patient. It must meet all the same requirements as an intermediate assessment.
- A933 On-call admission assessment
- Eligible for E082 Admission Assessment Premium if you’re the MRP. You can claim an on-call admission assessment if its the first hospital in-patient general assessment in 30 days if
- You’re a general practitioner or family physician participating in the hospital’s on-call roster (whether or not you’re on-call the day the service is provided).
- the admission is non-elective
- You’re the most responsible physician with respect to subsequent in-patient care.
- A100: General/Family physician emergency department assessment
- Use A100 when you give an emergency assessment (that satisfies as a minimum the requirements of an intermediate assessment) to a patient when you’re the patient’s general/family physician in an emergency department funded under an Emergency Department Alternative Funding Agreement (ED-AFA).
Substance Abuse Assessments
- A680: Initial assessment _ substance abuse
- C680: Initial assessment _ substance abuse _ subject to the same conditions as A680
- K680: Substance abuse _ extended assessment (per unit)
Focused Practice Assessment
- Focused practice assessment (FPA) is an assessment provided by a GP/FP if you have additional training and/or experience in sport medicine, allergy, pain management, sleep medicine, addiction medicine (including methadone) or care of the elderly (age 65 or older). The assessment must satisfy, at a minimum, all of the requirements of an intermediate assessment. No other consultation, assessment, visit or counselling service is eligible for payment when provided on the same day as any one of the FPA codes below.
- You should be prepared to provide to OHIP any documentation demonstrating training and/or experience (on request).
- A917: Sport medicine FPA
- A927: Allergy FPA
- A937: Pain management FPA
- A947: Sleep medicine FPA
- A957: Addiction medicine FPA
- A967: Care of the elderly FPA
Subsequent Visits
When seeing patients during rounds, you can claim MRP codes if you are in fact the MRP. If another physician claims the MRP premium as well and their billing is processed first by OHIP your claim will be adjusted accordingly to a lesser amount.
Special Visit Premiums aren’t eligible with subsequent visits since subsequent visits aren’t urgent.
As the MRP though, you can bill the E083 premium to your codes with the exception of C121 (C121 is billed after subsequent visits reach their maximum which makes it not eligible for the subsequent visit premium).
Subsequent visits
- C002: first five weeks
- C007: sixth to thirteenth week inclusive (maximum 3 per patient per week)
- C009: after thirteenth week (maximum 6 per patient per month)
- C121: Additional visits due to intercurrent illness
- C008: Concurrent care
- C010: Supportive care
- C882: Palliative care
Subsequent visits by the Most Responsible Physician (MRP)
- C122: day following the hospital admission assessment
- C123: second day following the hospital assessment
- C124: day of discharge
- C142: first subsequent visit by the MRP following transfer from an Intensive Care Area
- C143: second subsequent visit by the MRP following transfer from an Intensive Care Area
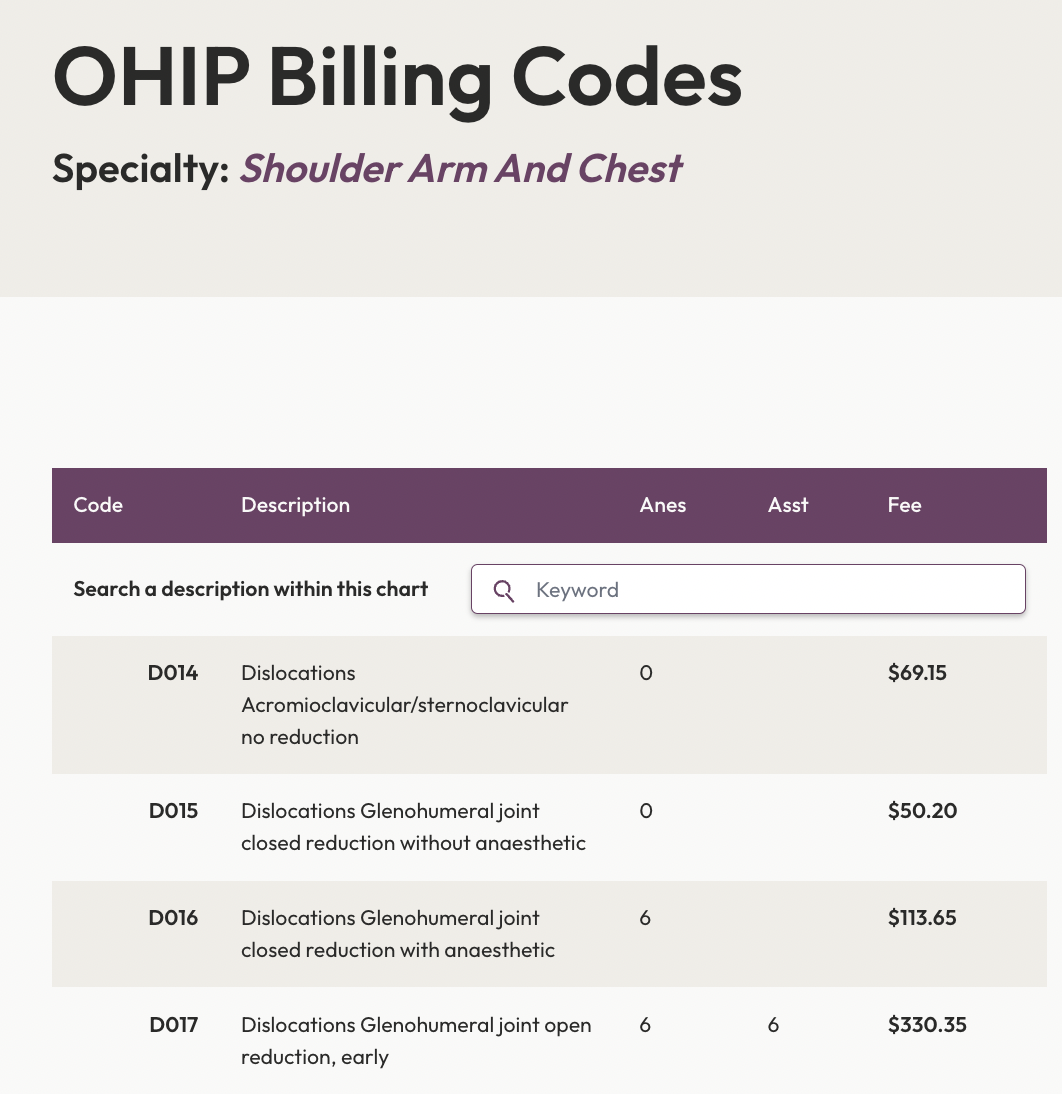
Search All OHIP Billing Codes
Search the Ontario Schedule of Medical Benefits electronically. We’ve digitized all the OHIP billing codes so you can easily find the most up to date billing rules and amounts.
Long Term Care Patients (nursing home, LTC within a hospital)
- W105: Consultation - Long-Term Care In-Patient
- W911: Special family and general practice consultation _ subject to the same conditions as A911
- W912: Comprehensive family and general practice consultation _ subject to the same conditions as A912
- W106: Repeat consultation
- W102: Admission assessment - Type 1
- W104: Admission assessment - Type 2
- W107: Admission assessment - Type 3
- W109: Periodic health visit
- W777: Intermediate assessment _ Pronouncement of death _ subject to the same conditions as A777
- W771: Certification of death _ subject to same conditions as A771
- W004: General re_assessment of patient in nursing home (per the Nursing Homes Act)
- W903: Pre_dental/pre_operative general assessment (maximum of 2 per 12 month period)
- W904: Pre_dental/pre_operative assessment
- W002: Chronic care or convalescent hospital - first 4 subsequent visits per patient per month (per visit)
- W001: Chronic care or convalescent hospital - additional subsequent visits (maximum 4 per patient per month) per visit
- W882: Chronic care or convalescent hospital - palliative care (see General Preamble GP34) per visit
- W003: Nursing home or home for the aged - first 2 subsequent visits per patient per month (per visit)
- W008: Nursing home or home for the aged - additional subsequent visits (maximum 2 per patient per month) per visit
- W872: Nursing home or home for the aged - palliative care (see General Preamble GP34) per visit
- W121: Additional visits due to intercurrent illness per visit
- W010: Monthly management fee (per patient per month)
- K124: Long term care/CCAC case (per unit)
- K705: Long term care high risk patient conference (per unit)
Non-Emergency Hospital In-Patient Services
As a Family Practitioner you can provide services to inpatients admitted to a facility. For these claims the Service Location Indicator should always be HIP (Hospital-in-patient), and the facility number should reflect Acute Care. While the requirements for consultations and assessments remain the same, for inpatient services make sure the service code prefix is C.
- C005 Consultation
- C911 Special family and general practice consultation
- subject to the same conditions as A911
- C912 Comprehensive family and general practice consultation
- subject to the same conditions as A912
- C945 Special palliative care consultation
- subject to the same conditions as A945
- C905 Limited consultation
- C006 Repeat consultation
- C003 General assessment
- C004 General re-assessment
- C813 Midwife-Requested Assessment
- subject to the same conditions as A813
- C815 Midwife-Requested Special Assessment
- subject to the same conditions as A815
- C816: Midwife-Requested Anaesthesiologist Assessment (MRAA)
- subject to the same conditions as A816
- C903: Pre-dental/pre-operative general assessment
- maximum of 2 per 12 month period
- C904: Pre-dental/pre-operative assessment
- C933: On-call admission assessment
- subject to the same conditions as A933
- C777: Intermediate assessment
- Pronouncement of death
Emergency Department H codes
H codes are only to be used for care provided in the emergency department.
- H065: Consultation in Emergency Medicine
- H105: In-patient interim admission orders
Monday - Friday
- H101: Minor assessment
- Monday to Friday - Daytime (08:00h to 17:00h)
- H104: Re-assessment
- Monday to Friday - Daytime (08:00h to 17:00h)
- H132: Comprehensive assessment and care
- Monday to Friday - Evenings (17:00h to 24:00h)
- H133: Multiple systems assessment
- Monday to Friday - Evenings (17:00h to 24:00h)
- H131: Minor assessment
- Monday to Friday - Evenings (17:00h to 24:00h)
- H134: Re-assessment
- Monday to Friday - Evenings (17:00h to 24:00h)
Weekends & Holidays
- H152: Comprehensive assessment and care
- Saturdays, Sundays and Holidays - Daytime and Evenings (08:00h to 24:00h)
- H153: Multiple systems assessment
- Saturdays, Sundays and Holidays - Daytime and Evenings (08:00h to 24:00h)
- H151: Minor assessment
- Saturdays, Sundays and Holidays - Daytime and Evenings (08:00h to 24:00h)
- H153: Multiple systems assessment
- Saturdays, Sundays and Holidays - Daytime and Evenings (08:00h to 24:00h)
- H151: Minor assessment
- Saturdays, Sundays and Holidays - Daytime and Evenings (08:00h to 24:00h)
- H154: Re-assessment
- Saturdays, Sundays and Holidays - Daytime and Evenings (08:00h to 24:00h)
Nights
- H122: Comprehensive assessment and care
- Nights (00:00h to 08:00h)
- H123: Multiple systems assessment
- Nights (00:00h to 08:00h)
- H121: Minor assessment
- Nights (00:00h to 08:00h)
- H124: Re-assessment
- Nights (00:00h to 08:00h)
Other
- H112: Other service rendered by Emergency Department Physician in premium hours
- Nights (00:00h to 08:00h)
- H113: Other service rendered by Emergency Department Physician in premium hours
- Daytime and evenings (08:00h to 24:00h) on Saturdays, Sundays or Holidays
- H100: Emergency department investigative ultrasound
Periodic Health Visit
A periodic health visit (including a primary or secondary school examination) is performed on a patient, after their second birthday, who presents and reveals no apparent physical or mental illness. The service must include an intermediate assessment, a level 2 paediatric assessment or a partial assessment focusing on age and gender appropriate history, physical examination, health screening and relevant counselling.
These are limited to one per patient per 12 month period:
- K017 child
- K130 adolescent
- K131 adult age 18 to 64 inclusive
- K132 adult 65 years of age and older
- A002 Enhanced 18 month well baby visit (must be 17-24 months of age)
- Claim A002 when you see a child between 17-24 months of age for all of the following services:
- Services defined as “well baby care.”
- Well baby care is a periodic assessment of a well newborn/infant during the first two years of life. It includes a complete examination with weight and measurements, and instructions to the parent(s) regarding health care.
- An 18 month age-appropriate developmental screen
- Review with the patient’s parent/guardian, legal representative or other caregiver of a brief standardized tool (completed by the patient’s parent/guardian, legal representative or other caregiver) that aids the identification of children at risk of a developmental disorder
- Services defined as “well baby care.”
- Claim A002 when you see a child between 17-24 months of age for all of the following services:
Eye examinations
- A115 Major eye examination
- As a General Practitioner you are eligible to provide a major eye exam once every 12 months for patients who have one of the following diagnosis:
- glaucoma
- cataract
- retinal disease
- amblyopia
- visual field defects
- corneal disease
- strabismus
- recurrent uveitis
- optic pathway disease
- As a General Practitioner you are eligible to provide a major eye exam once every 12 months for patients who have one of the following diagnosis:
OR
If your patient has a valid "request for eye examination requisition" completed by another physician or by a registered nurse holding an extended certificate of registration (RN(EC)).
- A110: Periodic oculo-visual assessment - aged 19 years and below
- A112: Periodic oculo-visual assessment - aged 65 years and above
A Periodic oculo-visual assessment is an examination of the eye and vision system that you give primarily to determine if your patient has a simple refractive error (defined as myopia, hypermetropia, presbyopia, anisometropia or astigmatism) for patients aged 19 or less, or aged 65 or more.
A110/A112 includes all components required to perform the assessment (ordinarily a history of the presenting complaint, past medical history, visual acuity examination, ocular mobility examination, slit lamp examination of the anterior segment, ophthalmoscopy, tonometry) advice and/or instruction to the patient and provision of a written refractive prescription if required.
- E077: Identification of patient for a major eye examination
- Identification of patient for a major eye examination, is the service of determining that a patient aged 20 to 64 inclusive has a medical condition (other than diabetes mellitus, glaucoma, cataract, retinal disease, amblyopia, visual field defects, corneal disease, strabismus, recurrent uveitis or optic pathway disease) requiring a major eye examination and providing such a patient with a completed requisition.
Midwife-requested Assessments & Delivery
- A813 Midwife-Requested Assessment (MRA)
- This is an assessment of a mother or newborn upon the written request of a midwife because of the complex, obscure or serious nature of the patient’s problem. Urgent or emergency requests may be initiated verbally but must subsequently be requested in writing.
- A815 Midwife-Requested Special Assessment (MRSA)
- Maximum 1 per patient, per pregnancy.
- A815 must include constituent elements of A813, specifically the common elements of a general assessment and you need to submit your findings/opinions and recommendations
- Verbally and in writing to both to the midwife and the patient’s primary care physician, if applicable.
It’s also payable if you’re a family physician or obstetrician. You can claim it for an assessment of a mother or newborn when, because of the very complex, obscure or serious nature of the problem, you spend at least 50 minutes in direct patient contact (exclusive of tests).
Be sure to include the start and stop times on your claim - to show you were with the patient for 50 minutes otherwise the claim won’t be paid and you’ll need to resubmit it under A813.
Additional help: How to Bill OHIP for Services Requested by an Aboriginal Midwife
Attending A Delivery
As a General Practitioner you are able to bill for being present at a delivery for high risk babies, as well as for newborn care, initial visits and subsequent visits. The following fee codes are eligible:
- H007 Attendance at maternal delivery for care of high risk baby(ies)
- You can only claim H007 if you haven’t billed for any other services at the time of the delivery.
- You need to be present for the entire delivery.
- It includes an assessment of the newborn after delivery.
- H001 Newborn care in hospital and/or home
- H002 Initial visit (per baby)
- H003 Subsequent visit
Certification of Death
- A771, C771 Certification of death
- You should only claim A771 (outpatient) or C771 (inpatient) if you are the physician who personally completes the death certificate on a patient who has been pronounced dead by another physician, medical resident or other authorized health professional.
- Make sure to include a diagnostic code for the underlying cause of death (that matches what’s been recorded on the death certificate). A771 and C771 includes any counselling you may have given to relatives during the same visit.
- If you're billing A902, A777 or C777 then you can't bill 771 as these fee codes already include completing the certificate.
- A777 Intermediate assessment: Pronouncement of death
- Use A777 if you have to pronounce a patient dead in a location other than in the patient’s home. It includes any counselling you may have given to relatives during the same visit as well as the completion of the death certificate.
- A902: House call assessment (Pronouncement of death in the home)
- When you pronounce a patient dead in their home you’d bill A902. It includes the death certificate and the counselling of any relatives during the same visit.
Other Miscellaneous GP Fee Codes
- K623: Application for psychiatric assessment
- K624: Certification of involuntary admission
- K629: All other re_certification(s) of involuntary admission including completion of appropriate forms
- K682:Opioid Agonist Maintenance Program monthly management fee - intensive, per month
- K684 - Opioid Agonist Maintenance Program team premium, per month, to K682 or K683
- K683: Opioid Agonist Maintenance Program monthly management fee - maintenance, per month
- K684 - Opioid Agonist Maintenance Program team premium, per month, to K682 or K683
- K002: Family meeting, caregiver interview
- K005: Primary mental health care – Individual care
- K007: Psychotherapy - Individual care
- K013: Counselling - Individual care
- K014: Counselling for transplant recipients, donors or families of recipients and donors
- K015: Counselling of relatives - on behalf of catastrophically or terminally ill patient
- K032: Specific neurocognitive assessment
- K040: Group counselling
- K121: Hospital in-patient case conference
- K035: Mandatory reporting of medical condition to the Ontario Ministry of Transportation
- K038: Completion of Long-Term Care health report form
- K070: Home care application
- K730: Physician to physician telephone consultation - Referring physician
- K731: Physician to physician telephone consultation - Consultant physician
- K732: CritiCall telephone consultation - Referring physician
- K738: Physician to physician e-consultation – Referring physician
- K033: Counselling individual care - additional units per patient per provider per 12 month period (per unit)
- K041: Group counselling - 2 or more persons - additional units where any group member has received 3 or more units of any counselling paid under codes K013 and K040 combined per provider per 12 month period (per unit)
- K140: Chronic disease shared appointment - 2 patients (per unit)
- K141: Chronic disease shared appointment - 3 patients (per unit)
- K142: Chronic disease shared appointment - 4 patients (per unit)
- K143: Chronic disease shared appointment - 5 patients (per unit)
- K144: Chronic disease shared appointment - 6 to 12 patients (per unit)
- K019: Psychotherapy - Group 2 people (per unit)
- K020: Psychotherapy - Group 3 people (per unit)
- K012: Psychotherapy - Group 3 people (per unit)
- K024: Psychotherapy - Group 5 people (per unit)
- K025: Psychotherapy - Group 6 to 12 people (per unit)
- K010: Psychotherapy - additional units per member (maximum 6 units per patient per day)
- K004: Psychotherapy - Family (2 or more family members in attendance at the same time) per unit
- K006: Hypnotherapy - Individual care
- K887: CTO initiation including completion of the CTO form and all preceding CTO services directly related to CTO initiation (per unit)
- K888: CTO supervision including all associated CTO services except those related to initiation or renewal (per unit)
- K889: CTO renewal including completion of the CTO form and all preceding CTO services directly related to CTO renewal (per unit)
- K003: Interviews with Children's Aid Society (CAS) or legal guardian on be half of the patient in accordance with the Health Care Consent Act conducted for a purpose other than to obtain consent (per unit)
- K008: Diagnostic interview and/or counselling with child and/or parent for psychological problem or learning disabilities (per unit)
- K708: MCC Participant, per patient
- K709: MCC Chairperson, per patient
- K710: MCC Radiologist Participant, per patient
- K700: Palliative care out_patient case conference (per unit)
- K704: Paediatric out_patient case conference (per unit)
- K701: Mental health out_patient case conference (per unit)
- K702: Bariatric out_patient case conference (per unit)
- K703: Geriatric out_patient case (per unit)
- K707: Chronic pain out_patient case conference (per unit)
- K706: Convalescent care program case conference
- K022: HIV primary care (per unit)
- K037: Fibromyalgia/chronic fatigue syndrome care (per unit)
- K023: Palliative care support (per unit)
- K106: Genetic assessment
- K028: STD management
- K029: Insulin therapy support (ITS)
- K030: Diabetic Management Assessment
- Q040: Diabetes management incentive
- K090: Pre_operative medical management of a bariatric surgery patient in a Bariatric RATC
- K091: Post_operative monthly management of a bariatric surgery patient in a Bariatric RATC
(E079 - Initial discussion with patient, to eligible services) - K039: Smoking cessation follow-up visit
- K018: Sexual assault examination - female
- K021: Sexual assault examination - male
- K026: Certification of Medical Eligibility for OHCAP
- K027: Certification of Medical Eligibility for OHCAP _ includes only completion of Application for OHCAP _ Physician's Form without an associated consultation or visit on the same day.
- K031: Completion of Form 1 _ Physician report in accordance with the Mandatory Blood Testing Act
- K071: Acute home care supervision (first 8 weeks following admission to the home care program)
- K072: Chronic home care supervision (after the 8th week following admission to the home care program)
- K036: Completion of northern health travel grant application form
- K034: Telephone reporting _ specified reportable disease to a MOH
- K399: Clinical interpretation by an immunologist
OHIP Premiums
- E082: Admission Assessment by the Most Responsible Physician (MRP) Premium (adds a 30% premium to the assessment code billed with this (Consultations, Assessments, etc).
- E083: Subsequent visit by the MRP premium (adds a 30% premium to the subsequent visit code).
- E084: Saturday, Sunday or Holiday subsequent visit by the Most Responsible Physician (MRP), to subsequent visits and C122, C123, C124, C142, C143, C882 or C982 (adds a 45% premium to the subsequent visit code if provided on Saturdays, Sundays and holidays).
Special Visit Premiums
OHIP special visit premiums are bonuses for working after-office hours. There’s 3 scenarios in which they apply:
| Travel Premium | First Patient Seen | Additional Person(s) Seen |
| When you travel from any place other than the hospital where the service is performed. | Applies only to your first patient. (If your shift goes past midnight, you can bill it again). | Applies to each additional patient after you’ve billed your first patient. |
They are categorized into 5 different time brackets:
| Weekdays | Mon - Fri (sacrifice of office hours) | Evenings (Mon - Fri) | Weekends & Holidays | Nights |
|---|---|---|---|---|
| 07:00 – 17:00 | 07:00 – 17:00 | 17:00 – 24:00 | 07:00 – 24:00 | 0:00 – 7:00 |
Special Visit Premiums Requirements
As a GP you’re eligible to add the following Special Visit Premiums to any non-elective (urgent and emergent) consults and assessments.
Guidelines:
- You can’t use them for routine rounds (as rounds are planned).
- You cannot claim them for visits to admit elective patients.
- They don’t apply to any subsequent hospital inpatient visits.
- You need to include the Visit fees and premiums on the same claim.
Emergency Department
| Weekdays | Mon - Fri (sacrifice of office hours) | Evenings (Mon - Fri) | Weekdays & Holidays | Nights | |
|---|---|---|---|---|---|
| Travel Premium | K960 : $36.40 Max. 2 | K961 : $36.40 Max. 2 | K962 : $36.40 Max. 2 | K963 : $36.40 Max. 6 | K964 : $36.40 Unlimited |
| First Person Seen | K990 : $20.00 Max. 1 | K992 : $40.00 Max. 1 | K994 : $60.00 Max. 1 | K998 : $75.00 Max. 1 | K996 : $100.00 Unlimited |
| Additional Person(s) Seen | K991: $20.00 Max. 9 | K993: $40.00 Max. 9 | K995: $60.00 Max. 9 | K999: $75.00 Max. 19 | K997: $100.00 Unlimited |
Hospital Out-Patient Department
| Weekdays | Mon. – Fri. “Sacrifice of Office hours” | Evenings – Mon. – Fri. | Weekends & Holidays | Nights | |
| Travel Premium | U960 : $36.40 Max. 2 | U961 : $36.40 Max. 2 | U962 : $36.40 Max. 2 | U963 : $36.40 Max. 6 | U964 : $36.40 Unlimited |
| First Person Seen | U990 : $20.00 Max. 1 | U992 : $40.00 Max. 1 | U994 : $60.00 Max. 1 | U998 : $75.00 Max. 1 | U996 : $100.00 Unlimited |
| Additional Person(s) Seen | U991: $20.00 Max. 9 | U993: $40.00 Max. 9 | U995: $60.00 Max. 9 | U999: $75.00 Max. 19 | U997: $100.00 Unlimited |
Hospital In-Patient
| Weekdays | Mon. – Fri. “Sacrifice of Office hours” | Evenings Mon. – Fri. | Weekends & Holidays | Nights | |
| Travel Premium | C960 : $36.40 Max. 2 | C961 : $36.40 Max. 2 | C962 : $36.40 Max. 2 | C963 : $36.40 Max. 6 | C964 : $36.40 Unlimited |
| First Person Seen | C990 : $20.00 Max. 1 | C992 : $40.00 Max. 1 | C994 : $60.00 Max. 1 | C986 : $75.00 Max. 1 | C996 : $100.00 Unlimited |
| Additional Person(s) Seen | C991: $20.00 Max. 9 | C993: $40.00 Max. 9 | C995: $60.00 Max. 9 | C987: $75.00 Max. 19 | U997: $100.00 Unlimited |
Long Term Care Institution
| Weekdays | Mon. – Fri. “Sacrifice of Office hours” | Evenings Mon. – Fri. | Weekends & Holidays | Nights | |
| Travel Premium | W960 : $36.40 Max. 2 | W961 : $36.40 Max. 2 | W962 : $36.40 Max. 2 | W963 : $36.40 Max. 6 | W964 : $36.40 Unlimited |
| First Person Seen | W990 : $20.00 Max. 1 | W992 : $40.00 Max. 1 | W994 : $60.00 Max. 1 | W998 : $75.00 Max. 1 | W996 : $100.00 Unlimited |
| Additional Person(s) Seen | W991: $20.00 Max. 9 | W993: $40.00 Max. 9 | W995: $60.00 Max. 9 | W999: $75.00 Max. 19 | W997: $100.00 Unlimited |
Special Visit to a Patient’s Home
(Excluding Long-Term Care Institutions).
| Weekdays – Both Elective & non-elective | Mon.-Fri. “Sacrifice of Office hours” non-elective | Evenings Mon.-Fri. non-elective | Weekends & Holidays – non-elective | Nights – non-elective | |
| Travel Premium | B960 : $36.40 Max. 2 | B961 : $36.40 Max. 2 | B962 : $36.40 Max. 2 | B963 : $36.40 Max. 6 | B964 : $36.40 Unlimited |
| First Person Seen | B990 : $27.50 Max. 10 | B992 : $44.00 Max. 10 | B994 : $66.00 Max. 10 | B993 : $$82.50 Max. 20 | B996 : $110.00 Unlimited |
Palliative Care Home Visit
| Weekdays | Mon.-Fri. “Sacrifice of Office hours” | Evenings Mon.-Fri. | Weekends & Holidays | Nights | |
| Travel Premium | B966 : $36.40 Unlimited | B966 : $36.40 Unlimited | B966 : $36.40 Unlimited | B966 : $36.40 Unlimited | B966 : $36.40 Unlimited |
| First Person Seen | B998 : $82.50 Unlimited | B998 : $82.50 Unlimited | B998 : $82.50 Unlimited | B998 : $82.50 Unlimited | B997 : $110.00 Unlimited |
Physician Office
| Weekdays | Evenings Mon. – Fri. | Weekends & Holidays | Nights | |
| Travel Premium | A960 : $36.40 Max.. 1 | A962 : $36.40 Max.. 1 | A963 : $36.40 Max.. 1 | A964 : $36.40 Unlimited |
| First Person Seen | A990 : $20.00 Max.1 | A994 : $60.00 Max.1 | A998 : $75.00 Max.1 | A996 : $100.00 Unlimited |
Other (non-professional setting not listed)
| Weekdays | Mon.-Fri. “Sacrifice of Office hours” | Evenings Mon.-Fri. | Weekends & Holidays | Nights | |
| Travel Premium | Q960 : $36.40 Max. 1 | Q961 : $36.40 Max. 1 | Q962 : $36.40 Max. 1 | Q963 : $36.40 Max. 1 | Q964 : $36.40 Unlimited |
| First Person Seen | Q990 : $20.00 Max. 1 | Q992 : $40.00 Max. 1 | Q994 : $60.00 Max. 1 | Q998 : $75.00 Max. 1 | Q996 : $100.00 Max. 1 |
Geriatric Home Visit
| Weekdays | Mon.-Fri. “Sacrifice of Office hours” | Evenings Mon.-Fri. | Weekends & Holidays | Nights | |
| Travel Premium | B986 : $36.40 Unlimited | B986 : $36.40 Unlimited | B986 : $36.40 Unlimited | B986 : $36.40 Unlimited | B986 : $36.40 Unlimited |
| First Person Seen | B988 : $82.50 Unlimited | B988 : $82.50 Unlimited | B988 : $82.50 Unlimited | B988 : $82.50 Unlimited | B987 : $110.00 Unlimited |
OTN Virtual Care in Ontario
Since OHIP doesn’t insure Telehealth services directly (except for the current COVID-19 k-codes), in order to get paid for your virtual visits in Ontario you need to first register with OTN - the government-funded non-profit that was created to expand the use of telemedicine across Ontario.
Submitting claims is relevantly the same as OHIP since you do submit claims through your billing service to OHIP. The only difference is that they are actually paid by OTN, who reimburses OHIP for your services.
Once registered with OTN there are two types of video visits that you can use to speak with patients, a hosted video visit or direct-to-patient video visit.
Hosted Video (Tracking code B103A)
- A Hosted Video Visit is when you speak with a patient who is currently at a patient host site. A patient host site is an organization that provides patients with an on-site location with videoconferencing technology and, in some cases, clinical support services (nursing support, diagnostics through peripheral devices).
Direct-to-patient Video (Tracking code B203A)
- A direct-to-patient video visit is when you speak with a patient who is either at their home or any other location besides a patient host site. This includes situations where your patient schedules and manages the encounter independently using their own technology, or where an organization provides support resources (e.g. access to technology).
How to submit a Virtual Care Claim
Submitting claims for virtual care is fairly easy, all you need to do is:
- Select the appropriate OHIP fee code; you can use anything except excluded fee codes.
- The Appropriate B-code for OTN tracking (B103A or B203A)
- Set the SLI location of your claim to ‘Ontario Telemedicine Network (OTN).’
When creating claims on Dr.Bill keep in mind that the OHIP fee code and the service code need to be on the same encounter (as shown below in our example).
WCB Claims
You get paid for both the insured insurances you provide and for reports, there are two different ways to submit claims:
- Insured Services: Submit a claim to OHIP like you normally would except on the claim you’ll indicate “WCB.” OHIP will then pay you for your services and bill WSIB accordingly. If you’re using Dr.Bill, select WCB at the top of the claim instead of OHIP like this:
- WSIB Forms: When you fill out a form, you bill WSIB. You need to upload these claims directly to WSIB through the online portal Telus Health. These claims have different fee codes than OHIP, which outline which form you’re using.
Final Takeaway:
On Dr.Bill you have the option of “starring” your most commonly used billing codes. That way, they’ll appear at the top for easy-searching.
If you have any questions about which fee codes to use contact our team and let us know the exact scenario.






