Unlike other specialties, there are a variety of MSP fee codes available for psychiatry. Not only are there consultations and assessments for hospitals, office, emergency, and home visits but there are also fee codes for giving advice, patient management and psychotherapy.
Knowing everything that’s available to bill within psychiatry will help maximize your claims by making sure you’re submitting the proper fee codes and getting paid for everything you do.
In an attempt to help make sure you’re billing properly, while reducing common rejections, we’ve put together this psychiatry billing guide for a quick reference of what fee codes are available.
General Consultation Guidelines
-
You can bill consults once every 6 months. If you need to bill a consult earlier than 6 months leave a note in the notes section of the claim with the reason why. The diagnosis must be different from the previous consult billed and unrelated to the last issue.
-
If your billing for the same illness within 6 months then bill a repeat consultation.
-
If, in your judgment, a consultation doesn’t warrant a full consultative fee then bill it as a repeat consultation.
-
Make sure you’ve added a referring physician to your claim. If the referral is unknown then use 99993 (however, MSP may ask for this physician’s name at a later date so it’s usually best to find out the name and add it to your claim as soon as you can).
Adult Psychiatry Fee Codes (ages 18-74)
- Psychiatry 00605: Emergency visit
- Not paid in addition to out-of-office hours premiums.
- Claim must include Start and End times.
- Psychiatry 00607: Visit, Office
- Psychiatry 00608: Visit, Hospital
- Psychiatry 00609: Visit, Home
- Psychiatry Consultation 00610: Private Office or Hospital Out-patient.
- Psychiatry Consultation 00615: Hospital/institution inpatient or home visit.
- Psychiatry 00625: Repeat consultation
Medical billing in BC is confusing and can often be overwhelming. To help out, check out our complete MSP guide that walks you through each step of medical billing – from the general teleplan process to maximizing your claims and using mobile billing.
Geriatric Psychiatry Fee Codes (ages 75 and older)
Psychiatry 00613: Geriatric Consultation
Psychiatry 00614: Repeat Geriatric Consultation
Child Psychiatry Fee Codes (17 years of age and younger)
Psychiatry 00622: Consultation (emotionally disturbed child)
Psychiatry 00626: Repeat Consultation (emotionally disturbed child)
Psychiatry 00623: Emotionally Disturbed Family
-
Must include three or more members.
Psychiatry 00627: Emotionally disturbed family – repeat consultation
Psychotherapy Timed Fee Codes:
Typically, there’s a lot of refusals with psychotherapy timed fee codes due to mistakes in selecting the time. Remember that the fee code you select has to match the amount of time you’re billing for.
For example, if you select 00630 (which has a time description of 1/2 hr) then your start and end times need to be a 1/2 hr, for example from 12:00pm – 12:30pm.
In our experience, a lot of physicians add a start time but no end time. MSP requires both a start and end time for the claim to be paid.
Psychiatry 00630: Psychotherapy individual (off.,out-patient) per 1/2 hr
Psychiatry 00631: Psychotherapy individual (off.,out-patient) per 3/4 hr hr
Psychiatry 00632: Psycho
therapy individual (off.,out-patient) per hour
Psychiatry 00650: Psychotherapy individual (hosp or institut) per 1/2 hr
Psychiatry 00651: Psychotherapy individual (hosp or institut) per 3/4 hr
Psychiatry 00652: Psychotherapy individual (hosp or institut) per 1 hr
Family Psychotherapy Billing Codes:
In order to bill family psychotherapy fee codes you need to have at least 2 members. Make sure you select the correct fee code that represents the amount of time you spent with the family (i.g. ½, 1 hr etc.) Don’t forget to add a start and end time that matches the fee code times.
Psychiatry 00633: Psychotherapy family per 1/2 hr
Psychiatry 00635: Psychotherapy family per 3/4 hr
Psychiatry 00636: Psychotherapy family per hour
Psychiatry 00638: Psychotherapy family per 1 1/4 hr
**A note record is required for sessions longer than one hour.
Psychiatry 00639: Psychotherapy family per 1 1/2 hr
** A note record is required for sessions longer than one hour.
Group Psychotherapy Billing Codes:
When you’re billing for group psychotherapy, you need to submit a separate claim for each patient. On each claim, make sure you add the start and end times (without those times your claim will be refused).
If you and another therapist are working in a group of 8 or more patients, then you’ll need to divide the patients for claim purposes (i.e. you both cannot submit claims for the same patients). Each claim should then indicate “co-therapy” and also identify the other co-therapist.
When a group psychotherapy session goes beyond 2 hours, or involved more than 20 patients, you need to leave a note in the MSP note section of the claim with a brief explanation of why.
Group Psychotherapy 00663: Three Patients, per patients.
Group Psychotherapy 00664: Four Patients, per patients.
Group Psychotherapy 00665: Five Patients, per patients.
Group Psychotherapy 00666: Six Patients, per patients.
Group Psychotherapy 00667: Seven Patients, per patient.
Group Psychotherapy 00668: Eight Patients, per patient.
Group Psychotherapy 00669: Nine Patients, per patient.
Group Psychotherapy 00670: Ten Patients, per patient.
Group Psychotherapy 00671: 11 Patients, per patient.
Group Psychotherapy 00672: 12 Patients, per patient.
Group Psychotherapy 00673: 13 Patients, per patient.
Group Psychotherapy 00674: 14 Patients, per patient.
Group Psychotherapy 00675: 15 Patients, per patient.
Group Psychotherapy 00676: 16 Patients, per patient.
Group Psychotherapy 00677: 17 Patients, per patient.
Group Psychotherapy 00678: 18 Patients, per patient.
Group Psychotherapy 00679: 19 Patients, per patient.
Group Psychotherapy 00680
: 20 Patients, per patient.
Group Psychotherapy 00681: Greater than 20 Patients, per patient.
Miscellaneous Psychiatry Fee Codes
Psychiatry 00699: Miscellaneous
You can submit claims under the 00699 miscellaneous fee code only if you meet the following criteria:
-
An estimate of an appropriate fee, with rationale for the level of that fee. It’s best to contact our billing agents so that we can manually input the amount you’d like to create the miscellaneous claim for.
-
Sufficient documentation of the services (such as the operative report) to substantiate the claim.
00066 Mental Ill – Health Documentation Completion of B.C. Mental Health Act Forms 3, 4 or 6, on previously assessed or treated cases.
00065 Mental Ill – Health Investigation Investigation with completion of B.C. Mental Health Act Forms 3, 4 or 6 (fee per doctor).
00067 Mental Ill – Health Investigation Investigation with cancellation of B.C. Mental Health Act Forms 4 or 6, and subsequent voluntary treatment status.
Telephone and Conference Psychiatry Fee Codes
Psychiatry 00645: Patient Management Conference. 3rd parties, per 1/4 hr.
-
You cannot exceed the maximum of 4 hours per patient, per calendar year.
-
Not payable unless you’ve seen your patient sometime in the past 180 days.
-
If 4-hour maximum has been exceeded try billing 10004 (Spec multidisciplinary conferencing for complex pt).
-
When billing more than one unit, if the times are consecutive, it’s best to bill everything on one claim so MSP doesn’t refuse it, thinking it’s a duplicate. Remember that Dr.Bill will automatically calculate the units to the appropriate amount.
-
00645 isn’t part of the reciprocal agreement, therefore, you can’t claim it for out of province patients.
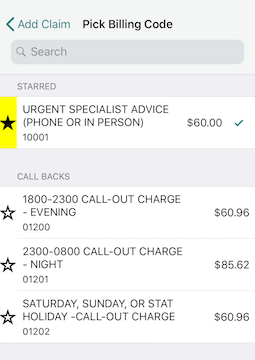
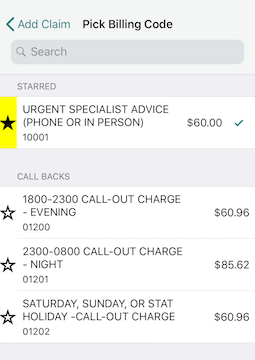
Urgent Specialist Advice 10001: (phone or in person).
You can only bill 10001 for patients you haven’t previously seen for the same condition.
If you have previously seen this patient for the same condition, within the preceding 180 days, then you’re not eligible to bill for it. An unrelated diagnosis must be billed in those circumstances or possibly 10004 if it was for conferencing.
Specialist Multidisciplinary Conferencing for Complex Patient 10004.
Any specialist involved in the conference is eligible to bill for it. Each person must create their own claim. You can bill up to a maximum of 4 units, per patient, per day. However, you can only claim a total of 16 units per patient, per year.
10004 isn’t part of the reciprocal agreement, therefore, you can’t claim it for out of province patients.
Telehealth Psychiatry Fee Codes
You can bill telehealth whenever you treat or speak to a patient through an approved site via video.
Telehealth Guidelines
You can bill telehealth fee codes once per patient, per day. If for some reason you need to bill more than one service leave a note in the notes section of the claim explaining why. Don’t forget to include the start and end times.
All telehealth fee codes follow the same rules as face-to-face consultations or repeated consultations. This means that for any session that goes longer than 1 hour, you need to leave a brief note explaining why in the notes section of the claim.
If after providing a Telehealth consultation you realize you need to examine the patient in person, then the subsequent visit is claimed as a limited consult (unless more than 6 months have passed from the initial consult).
If the telehealth video is interrupted due to technical failure then just submit a claim under 00699.
Psychiatry 60610: Telehealth Consultation Psychiatry (ages 18-74).
Psychiatry 60613: Telehealth Geriatric Consult Psychiatry (75 yrs or older).
Psychiatry 60622: Telehealth Consult Emotionally Disturbed child (17 and under).
Psychiatry 60625: Telehealth Repeat/Limited Consult Psychiatry.
Psychiatry 60614: Telehealth Repeat/Limited
Geriatric Consult Psychiatry.
Psychiatry 60626: Telehealth Repeat/Limited Geriatric Consult Emotionally.
Psychiatry 60607: Telehealth Subsequent Office Visit Psychiatry
Psychiatry 60608: Telehealth Hospital In-patient Visit Psychiatry
Psychiatry 60630: Individual Telehealth Psychiatric Treatment, 1/2 HR.
Psychiatry 60631: Individual Telehealth Psychiatric treatment, 3/4 HR.
Psychiatry 60632: Individual Telehealth Psychiatric Treatment, 1 HR.
Psychiatry 60633: Family/Conjoint Telehealth Therapy – per 1/2 HR.
Psychiatry 60635: Family/Conjoint Telehealth Therapy – per 3/4 HR.
Psychiatry 60636: Family/Conjoint Telehealth Therapy – per 1 HR.
Psychiatry 60638: Family/Conjoint Telehealth Therapy – per 1 1/4 HR.
Psychiatry 60639: Family/Conjoint Telehealth Therapy – per 1 1/2 HR.
Psychiatry 60624: Telehealth Evaluation Interview with a family member, 1/2 HR.
-
The call has to be at least 15 minutes or more.
-
Payable in addition to other services when performed consecutively, not concurrently.
-
Maximum of one hour (4 units) may be claimed per patient, per day.
-
Payable when the interview is in person or by telephone.
-
Start and end times must be included in the time fields (otherwise your claim will get refused).
-
When billing more than one unit, if the times are consecutive, it’s best to bill everything on one claim so MSP doesn’t refuse it thinking it’s a duplicate. Remember that Dr.Bill will automatically calculate the units to the appropriate amount.
Psychiatry 60645: Telehealth Patient Management Conference Psychiatry
-
Per 15 minutes or greater portion thereof.
-
Not to exceed a maximum of 4 hours per patient, per calendar year.
-
Not payable unless you’ve seen the patient in the past 180 days.
-
If multiple patients are discussed, claims should be consecutive, non-overlapping time periods.
Make sure you save a link to our MSP Psychiatry searchable database. You can search by billing code or keyword.
MSP Psychiatry Fee Code Lookup
Final Takeaway:
Remember you have the option of “starring” your most commonly used billing codes. That way, they’ll appear at the top for searching.
If you find you’re getting a lot of MSP rejections or would simply like to clarify something, don’t hesitate to get in touch with us.

Additional Reading
Dr. Nour Khatib left medical school for a finance career, but a persistent calling encouraged her to return years later and become an emergency physician.