Looking for help with anaesthesiology billing? Having a reference list of common fee codes on hand can go a long way towards saving you time and reducing your administrative workload. This fee listing includes codes for general and regional anaesthesiology procedures, resuscitation and critical care, monitored anaesthesia care, and any other medical procedure carried out by the anesthesiologist at the request of the attending physician. These fees are payable to all anesthesiologists, with the exception of consultations and continuing care by consultants, which are payable only to certified specialists in anesthesia.
Guidelines and Criteria:
MSP begins your billable time when you first enter the operating room for the purpose of providing anaesthetic. Your time ends when you leave and when the patient can be safely left in the care of nursing staff. While you are working, you should calculate your time in 15 minute increments or parts thereof – for example, if your final period of anaesthetic is 9 minutes, you would be able to bill for the full 15. Other guidelines to keep in mind include:
Routine P.A.R (Post-Anesthetic Recovery) care
Any time you spend with the patient after your anaesthetic in the P.A.R for routine problems should be billed at the same rate as the anesthetic and included in the procedural fee for the anaesthesia.
Additional Procedures
When you perform more than one surgical, diagnostic, or therapeutic procedure during the same session, the rate for your total anaesthetic time will be the rate for whichever procedure has the highest procedural rate.
Anaesthetic Procedural Fees
The procedural fee for your anaesthesia time covers all of the services you’ll render during the procedure, except for the anaesthetic procedural fee modifiers and acute pain management. It is calculated by multiplying the intensity/complexity level of the anaesthesia by the anesthetic time per 15 minute interval.
Anaesthetic Procedural Fee Modifiers
These modifiers pay you an additional amount over and above your anesthetic procedural fee. They apply to all of your general, regional, and monitored anesthetic care for any surgical, therapeutic, and/or diagnostic procedures you might perform. You cannot use them with diagnostic or therapeutic anaesthesiology fees.
Keep in mind that some modifiers may require additional information. For example, when billing the modifier code 00169, your claim must include a note indicating the patient’s body mass index (eg. BMI 35.5)
Consultations and Anaesthetic Assessments
These are not payable in addition to critical care fees. However, if they are done prior to surgery (for example, if you see a patient a week before a procedure to consult with them on their surgical risk) then you would be able to bill for this.
Consultations are allowed once per 6-month period. All types of consultations (as outlined below) need to have been referred to you by a physician or nurse practitioner.
| Procedure | Expectations | Allowable Frequency |
| Consultation | Full medical history required, must be referred to you by another physician or nurse practitioner. | Once per 6 month period |
| Repeat Consultation | Full medical history required, must pertain to different medical issue than previous consultation. Must be referred to you by another physician or nurse practitioner. | Once per 30 day period, but only for a completely different medical issue |
| Limited Consultation | Full medical history not required. Must be referred to you by another physician or nurse practitioner. | Once per 30 day period, |
| Complete Examination | Full medical history required; less time spent with the patient than a consultation. Does not require a referral and can be both a scheduled appointment or emergency visit. | Once every 12 month period (if you need to bill this twice for a patient within 12 months you need to have a note explaining why). |
Acute Pain Management
These fee codes apply to any services you might provide relating to the management of what is deemed ‘acute’ pain in certain categories of patients. These include post-operative surgical patients, surgical patients who do not necessarily undergo surgery but have problems with acute pain, and medical patients who have acute pain problems. These listings are not applicable to pain management during labour.
All acute pain management billing codes can be used in combination with the out-of-office service charges and continuing care surcharges.
The acute pain management codes cannot be applied to claims for critical care fee items 01088, 01412, 01413, 01422, 01423, 01432, 01433, 01442 and 01443 if the anesthesiologist trying to claim them is capable of acute pain management.
Diagnostic/Therapeutic Fees
Anaesthesia fees for diagnostic and therapeutic services can be billed but are not eligible for the out-of-office or continuing care service charges. They are also not allowed to be used with anaesthetic procedural fee modifiers.
Dual Anesthesiologists
In some situations, providing care to a patient may require two anaesthesiologists to be present for the procedure. In this case, both doctors may charge their full fee – however, when billing MSP for these fees, both doctors need to support the need for these charges with a written statement.
If one anaesthesiologist takes over from another one, partially through a procedure, the total fee billable by both anesthesiologists should not exceed the fee that would have been billed had the procedure been performed by only one doctor (if the replacement did not occur).
Common Fee Codes:
Here’s an overview of some of the most commonly used codes:
Pre-Anesthetic Evaluation Fees:
01151: Pre-anaesthetic evaluation – standard
- Applicable to certified anesthesiologists only.
13052: Anaesthetic evaluation – non-certified anaesthetist
- Used for in-patient visits where a separate visit prior to the anaesthetic is required. If you’re performing a visit immediately prior to the anaesthetic, it will be paid using the anaesthetic intensity/complexity level of the procedure itself and 01151 – this code will not be paid in addition.
- Can also be used for out-patient visits where a separate visit for an anaesthetic assessment is required (such as in a pre-anesthetic clinic).
Consultations:
01015: Consultation, anaesthesia
- This code is used when a certified anaesthesiology specialist is requested for a patient assessment because of the complexity, obscurity, and/or seriousness of the case.
01115: Consultation – repeat/limited – anaesthesia
- This is used when a repeat consultation is necessary for the same condition within six months and done by the same consultant.
- It is also used for a limited consultation when in the opinion of the consultant the problem does not warrant 01015.
01016: Consultation, mgmt of complicated chronic pain
- This code is used in consultations for complex diagnostic and/or therapeutic chronic pain management problems that need a comprehensive history and a physical examination.
01116: Consultation – repeat or limited – diagnostic/pain mgmt
- Used when, in the opinion of the consultant, the diagnostic and/or therapeutic chronic pain management problem is of a more limited nature.
- If the same physician sees a patient for a consultation within six months of billing 01016 for the same problem, then they would also use this code.
01107: Office visit – anaesthesia
- This fee code applies to patient visits conducted in a private office setting where the physician has an increased overhead.
01155: Telehealth Anesthesiology Consultation:
- This is used for telehealth sessions conducted by a certified specialist in Anesthesiology because of the complexity, obscurity and/or seriousness of the case. Includes appropriate history and an appropriate physical examination, as well as a review of pertinent radiological and laboratory findings and a written report.
Visit / Evaluation:
01107: Office visit.
- Not paid with other listings.
01108: Hospital visit (weekday)
- Not paid with other listings.
- Applies only on weekdays, excluding statutory holidays.
- Out-of-Office Hour Premiums are not applicable.
01109: Hospital visit (Saturday, Sunday, or statutory holiday)
- Not paid with other listings
- Applies only on Saturday, Sunday, or statutory holidays
- Out-of-office Hour Premiums are not applicable
Call Outs & Continuing Care Premiums
A call out is a premium added when you are called from outside of the hospital to come and care for a patient. During weekdays the call must be placed prior to 8:00am or after 6:00pm. On weekends the call must be placed after 8:00am.
REMINDER: If you’re called during regular weekday hours you’d bill an emergency visit instead, which covers both the visit and the surcharge.
Continuing Care
If you have logged a Call Out charge and then continue to see additional patients you would be entitled to bill continuing care surcharges for each 30 minutes after the initial 30 minutes you spent with the patient you were initially called to see.
If you see multiple patients in a 30 minute block you would only log the continuing care on the last patient in that block but for the entire 30 minute period. You must also note CCFPP in the MSP note field to tell MSP that these patients were seen following your initial call out to the hospital.
Continuing Care Rules
Timing begins after the first 30 minutes for consultations, visits or anesthetic evaluations. Payment is based on one half-hour of care or major portion thereof (at least 15 mins.). This means that your first continuing care surcharge is only eligible after 45 minutes of continuous care (30 mins. for the refractory period plus the major portion of 15 minutes).
Timing for the continuing care premium is based on the total time spent providing continuous care, not the number of patients you see. For example, if you see 3 patients within 30 minutes then you would only add the continuing care premium on the last patient, but for the entire 30-minute duration.
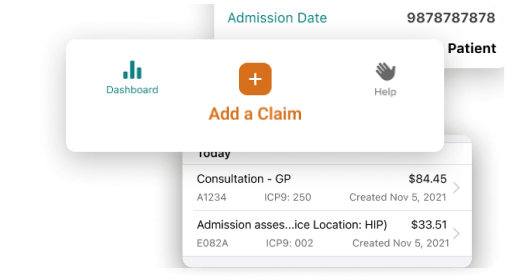
To apply these surcharges on Dr.Bill, log your consult or visit with the patient. On that claim toggle ‘Call Out & Continuing Care’. Don’t forget to enter the Call Time, Start Time & End Time for your encounter. Our app will automatically apply the correct Out of Office premiums to your claim.
Reminder: Only toggle Call-Out on the first patient, to show that it was the first. For the following claims just toggle Cont.Care. If you need to claim a call out on its own or aren’t using Dr.Bill then use the following fee codes:
Call Out Fee codes:
01200: Evening (call placed between 6:00pm and 11:00pm and service rendered between 1800 hours and 0800 hours)
01201: Night (call placed and service rendered between 11:00pm hours and 8:00am)
01202: Saturday, Sunday or Statutory Holiday (call placed between 8:00am and 11:00pm)
Continuing Care Surcharge Fee Codes (non-operative):
Billed in addition to visits and consultation fees.
01205: Evening (service rendered between 6:00pm and 11:00pm) – per half hour or major part there of
01206: Night (service rendered between 11:00pm hours and 8:00am) – per half hour or major part thereof
01207: Saturday, Sunday or Statutory Holiday (Service rendered between 8:00am and 11:00pm) – per half hour or major part thereof
Anesthetic Procedural Fees:
The anaesthetic intensity/complexity level will be listed in the schedule opposite the specific surgical, diagnostic and/or therapeutic procedure that you are providing to the patient. Anaesthetic intensity level/complexity time units are also indicated in the listing – these represent the different degrees of complexity and intensity for each procedure. Fees for your time are allocated in accordance to this intensity/complexity.
Intensity and Complexity Index Intensity/Complexity Fee:
For each 15 minute Level Code or part thereof.
Level 2: 01172
Level 3: 0117
Level 4: 01174
Level 5: 01175
Level 6: 01176
Level 7: 01177
Level 8: 01178
Level 9: 01179
Level 10: 01180
Level 11: 01181
01088: P.A.R. (Post-Anesthetic Recovery)
- Critical Care: your critical care time spent with the patient begins when the anesthetic finishes (for example, a post-operative abdominal aortic aneurysm on a ventilator).
- Resuscitation: used for life-threatening emergencies in the P.A.R. (e.g.: respiratory arrest in the recovery room requiring intubation).
Anesthetic Procedural Fee Modifiers:
These are fixed fees that are paid in addition to the basic anesthetic procedural fees – these give you additional compensation for performing anaesthesia in certain situations. They are not included in the anesthetic procedural fee for the application of 01080.
01059: Prone position
01065: Patients under 1 year of age
- Note: Not to be billed in addition to 01168.
01070: Controlled hypotension in neurosurgical anesthetic to lower mean blood pressure to 60 mm Hg or less, or the appropriate safe lower limit
01071: Thoracic epidural catheter insertion during anesthetic, to include initial injection and/or infusion set-up
01072: Lumbar epidural catheter insertion during anesthetic, to include initial injection and/or infusion set-up
01077: Pulmonary artery catheterization
01082: Axillary catheter insertion during anesthetic, to include initial injection and/or infusion set-up
01084: Intrapleural catheter insertion during anesthetic, to include initial injection and/or infusion set-up
01093: Spinal cord monitoring (interpretation of SSEP during anesthetic)
01096: Retrobulbar/peribulbar block administered by an anesthesiologist in conjunction with an anesthetic
01164: Patients 70 – 79 years of age
01165: Patients 80 years of age and over
01166: Sitting position where there is a danger of venous air embolism
01168: Neonates (less than 42 gestational weeks and/or 4000 grams or less)
01192: Awake intubation by any means in the patient with a suspected or proven difficult airway
- Note: Applicable only when airway score is 3 or 4.
01169: BMI ≥ 35 per 15 minutes or part thereof
- Restricted to certified specialists in anaesthesiology and payable only when fee items 01172, 01173, 01174, 01175, 01176, 01177, 01178, 01179, 01180, 01181, 01005, 01106, 01110, or 01111 are also payable.
- Applicable to all patients ≥ 19 years of age with a BMI ≥ 35 and to all patients < 19 years of age with a BMI ≥ 97th percentile adjusted for age and gender.
- You must provide the patient’s BMI in the claim note record and document it on the patient’s anesthetic record.
01080: In the following cases an additional 15% of the procedural fee will be paid:
- All patients (except cardiac surgery patients) who have an incapacitating, systemic disease which is a constant threat to life, or who are not expected to survive for 24 hours, i.e. ASA 4 or 5.
- Cardiac surgery patients who have emergency surgery, i.e. ASA 4E or 5E.
- Cardiac or transplant surgery patients who require an IABP or mechanical assist device.
- All cases where the surgical time as noted on the OR record is 8 hours or more. This includes cardiac surgery.
Diagnostic and Therapeutic Anesthetic:
These fees are for diagnostic and therapeutic procedures not associated with surgery. They are not eligible for out-of-office or continuing care service charges or procedural fee modifiers.
01124: Peripheral nerve block – single
01125: Peripheral nerve block – multiple
01135: Lumbar Epidural block
01140: single nerve Root or Facet Blocks ( Cervical )
01141: multiple nerve Root or Facet Blocks ( Cervical )
01142: single nerve Root or Facet Blocks (Thoracic)
01143: multiple nerve Root or Facet Blocks (Thoracic)
01144: single nerve Root or Facet Blocks (Lumbar)
01145: multiple nerve Root or Facet Blocks (Lumber)
- Note: Fee items 01140, 01141, 01142, 01143, 01144 and 01145 must be performed under medical imaging guidance (ultrasound, fluoroscopy or CT) with image capture.
Resuscitation by an Anesthesiologist:
01088: Resuscitation by an anesthesiologist, requiring continuous bedside care – per 15 minutes or part thereof
- Includes endotracheal intubation, cricothyroidotomy, chest tube drainage, monitoring, and pacemaker insertion.
- Consultation not paid in addition.
01090: Neonatal resuscitation by an anesthesiologist – per 15 minutes (or part thereof)
- Applicable where the Apgar score is 5 or less, as noted on the delivery record.
- Includes endotracheal intubation and/or umbilical vessel catheterization.
- Consultation not paid in addition
01091: Intubation requested by attending physician, with no responsibility for subsequent care.
- Applicable to removal and reinsertion of ET tube.
- Consultation not paid in addition
Obstetric Analgesia Fees:
01102: Insertion of epidural catheter. To include initial injection and/or set-up of infusion for analgesia during labour
Supervision of Labour Epidural Analgesia
01047: Medical Supervision of Labour Epidural Analgesia: Daytime (Monday to Friday, 0800-1800 hrs), per 5 minutes (or major portion thereof)
01048: Medical Supervision of Labour Epidural Analgesia: Evening (Monday to Friday, 1800-2300 hours), and Weekends (Saturday & Sunday, 0800-2300 hours) and Statutory Holidays (0800-2300 hours), per 5 minutes (or major portion thereof)
01049: Medical Supervision of Labour Epidural Analgesia: Night (Monday to Sunday, 2300-0800 hours), per 5 minutes (or major portion thereof)
- You are allowed to bill these fees concurrently with services provided to other patients, including concurrent payment of fee items 01047, 01048, 01049 for more than one patient.
- The fee items 01047, 01048, 01049 are payable to a maximum of 48 units per patient, per maternity.
Payment for labour epidurals begin immediately after the labour epidural catheter is inserted and continues until the earliest of the following:
- 4 hours duration of medical supervision (48 time units)
- Time of birth
- Time when payment begins for anesthetic care on the same patient related to c-section, complicated delivery, or surgical delivery.
Keep in mind that these fees also include payment for labour epidural analgesia top-ups and supervision visits. Exceptions include the reinsertion of a labour epidural catheter, which is payable under fee item 01102 and not considered part of the medical supervision period. Out-of-office premiums like call out charges and continuing care surcharges (both non-operative and anaesthesiology) are not payable.
The time period (e.g.: daytime, evening, night) that the medical supervision begins determines which fee item will be paid for the entire duration, even if the supervision time continues into a new time period – start and end times are required in the time field.
Acute Pain Management:
01013: Used for a consultation by a certified specialist in anesthesia for assessment of the patient for postoperative acute pain management. It can be used when the consultation is requested after admission and either prior to surgery or within 24 hours following the end of surgery.
01073: Hospital visit for supervision of epidural infusion to a maximum of 2 per day – per visit
- Note: Where more than 2 visits per day are necessary, an explanatory note in the claim note record is required.
01011: Patient controlled analgesia (PCA) – first day only (to include set up).
01012: Hospital visit for supervision of patient controlled analgesia during second and subsequent days, to a maximum of 2 visits per day – per visit.
- Where more than 2 visits per day are necessary, an explanatory note in the claim note record is required.
- 01012 is not payable on the same day as 01011.
01186: Major peripheral nerve block – single
01187: Major peripheral nerve block – multiple
For a complete breakdown of how medical billing works for Anesthesiologists in BC see our complete billing guide.
This article offers general information only and is not intended as legal, financial or other professional advice. A professional advisor should be consulted regarding your specific situation. While information presented is believed to be factual and current, its accuracy is not guaranteed and it should not be regarded as a complete analysis of the subjects discussed. All expressions of opinion reflect the judgment of the author(s) as of the date of publication and are subject to change. No endorsement of any third parties or their advice, opinions, information, products or services is expressly given or implied by RBC Ventures Inc. or its affiliates.
Features that fit your practice
Our software helps you save time, collaborate with ease and get expert support.






