In Ontario, if you’re a doctor working under the fee-for-service model then you are essentially a small business. This means you are responsible for submitting “invoices” of who you saw and what you did to the ministry of health.
The OHIP Claims Submission Process
Depending on what kind of program you're using, whether a billing component of an EMR / CMS or billing software, the specific workflow of submitting claims may differ.
Ultimately though, the general process is similar:
- You see a patient.
- You submit a claim to OHIP that outlines what service you provided, along with the diagnosis of your patient.
- OHIP reviews your claims and reimburses you if it’s approved.
OHIP Fee Codes
Each service you provide corresponds to a fee code with a specific dollar amount. OHIP fee codes are outlined by the Ministry of Health in the Schedule of Benefits.
There are over 6,000 services listed so it’s best if you use the online searchable database to easily find the service or code you’re looking for.
You can search by speciality, billing code or keyword.
How to Upload OHIP Claim Submissions
- Once you create a claim, you need to send it to OHIP in order to get paid.
- Claims are submitted through the medical claims electronic data transfer (MC EDT) system.
- The MC EDT system is currently the only way that claim data is sent to the Ontario Health ministry.
- Claim files must be submitted in a specific file format as outlined in the
Technical Specifications-Interface to Health Care Systems manual.
There are two options you can choose from when registering to submit claims:
1. MC EDT - Web Page
You can submit your claims directly online to OHIP by logging in on the MC EDT secure web page and uploading each claim.
However, you will still need third party software to create the correct claim file for submission, as the file needs to meet certain technical specifications.
2. MC EDT – Web Service
You can create your claims and upload them to OHIP through an authorized third-party billing software. This allows you to create and submit claims at the same time, and is a more automated system to submitting and receiving claim files.
With this option you’ll have more reporting tools such as:
- Remittance Advice Reports
- Claims Error Reports
- Designation to admin staff or third parties agents to submit and reconcile claims on your behalf (so you don’t have to go through every rejection and resubmit them yourself).
In order to use the MC EDT system you need to be an authorized user. Registration is easy as you can set up your account and connect it to your billing software all in one step.
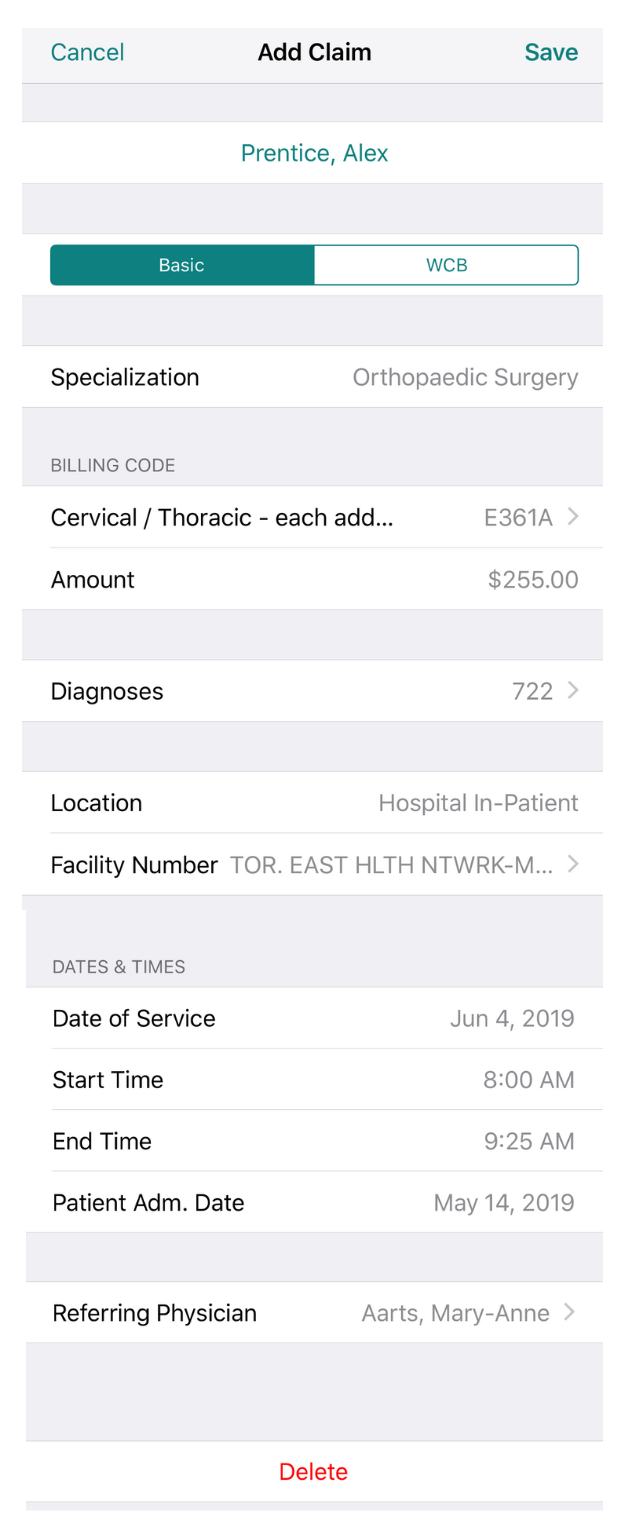
OHIP Claim Example
Here’s an example of an electronic claim, and everything that needs to be included in order for OHIP to approve the claim.
Patient: Alex Prentice
Speciality: Orthopaedic Surgery
Fee Code: E369A
Amount: $255
Diagnosis: 722
DOS: May 27th
Location: HP
Facility: 1302
Start & Stop Times: 8:00 am - 9:25am
Referring Physician: Mary-Anne Aarts
- Reminder: You have to include a diagnostic codes along with the fee code. Diagnostic codes are also outlined in the schedule of benefits.
The 4 Different Types of OHIP Claims
There are 4 different types of claims that you can submit for reimbursement.
1. OHIP Health Claims (HCP)
- OHIP Health Claims are regular claims submitted to OHIP for services provided to patients who have valid Ontario health insurance coverage.
HCP claims are your typical, everyday claims that are created based on the Fee codes outlined in the schedule of benefits.
In order to be paid your claim always needs to include:
- Your patient's information (in order to make sure they're eligible for insurance coverage for that service).
- The details of the service – which is done by including a fee code and a diagnostic code.
2. Reciprocal Medical Billing (RMB)
- RMB claims are claims for out of province patients who have valid Canadian Health insurance from another Canadian provincial/territorial health coverage plan.
All Provinces, and Territories, except Quebec, have entered an agreement to pay for insured services provided to residents of other provinces when a patient has a valid Provincial Health Registration Card from another province.
RMB claims are created exactly the same as regular claims (using the OHIP fee codes), just make sure you change the province when you add the patient into your billing software.
If your patient is from Quebec, you need to bill them privately (see: 3.Private Billing below). They will have to pay the invoice and then submit their own claim to Quebec for reimbursement.
3. Workplace Safety Insurance Board (WSIB)
- WSIB claims are created for patients who have been injured at work.
There are two ways that WSIB will reimburse you for your services; through the insured insurances you provide (using the regular OHIP fee codes) and for reports of the incident (using WSIB Fee Codes).
To submit claims to OHIP and WSIB you need to register with Telus Health here and follow the online instructions.
4. WSIB Insured Services:
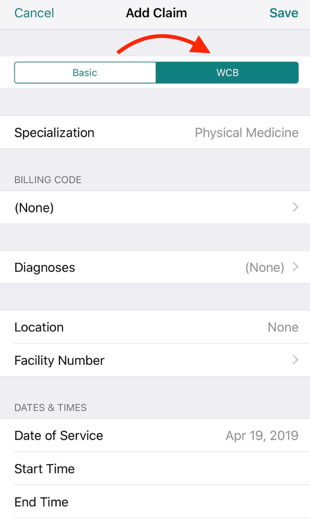
If order to submit a claim using OHIP fee codes, create a claim like you normally would but select WCB instead of OHIP. OHIP will then pay you for your services and bill WSIB accordingly. If you’re using Dr.Bill, select WCB at the top of the claim instead of ‘Basic’ like this:
5. WSIB Forms
When you see a patient who has been hurt at work sometime WSIB will ask you to fill out a report in addition to the claim you submitted. This report will be reimbursed directly through WSIB.
Report claims have their own
WSIB fee codes and need to be done directly through the online WSIB portal.
***Remember, whether you’re submitting claims through OHIP, or you’re uploading forms to the WSIB online portal, you need to register with WSIB first.
OHIP Claim Submission Deadlines
OHIP claim submissions run on a monthly cycle. All claims you submit until the 18th of each month will be processed for payment by the 15th of the next month.
When the 18th falls on a weekend or holiday, the deadline will be on the next business day. Claims received after the 18th of the month might get processed by the end of the month.
OHIP Claim Reports
-
Remittance Advice (RA) Report
The RA report is essentially your monthly report of claims that were approved and paid.
You'll get this report at the beginning of each month – usually between the 5th and 7th. (Payment will then be received for approved billings on the 15th business day).
-
Claims Error Report
Billing OHIP can result in having claims sent back with Claims Error Reports detailing various issues with submitted claims.
Use our searchable database to find the code from your Claims Error Report here:
Reconciliation and Payment
When a claim does get rejected or the payment is reduced, you can resubmit the claim and inquire to appeal the decision.
The Remittance Advice Inquiry form is used to inquire about these underpaid claims. This needs to be done within four months from the issue date of the RA report that detailed the claim in question.
Keep in mind that claims have to be submitted within six months of the original date of service.
Any billings submitted after that deadline will be rejected and become 'stale dated' claims.
How claim submission works on Dr.Bill
Dr.Bill is a platform used by 8000+ Canadian physicians to manage their billing.
We offer a smartphone app that lets you take a picture of a patient label and submit your claims in a few taps. You can then review your submissions and manage rejections on the web.
Doctors use our system alongside their EMRs – submitting their billings as they work and never missing a claim again.
Our team of in-house OHIP billing agents are always here to help. They are truly experts at what they do so we strongly encourage reaching out anytime you’ve got questions. We are not only a software but a service too.
If you’re looking for more information on how to automate the billing process check out our Ultimate OHIP Billing Guide.

Claim Your $150 Credit!
Get a $150 Credit when you sign up for Dr.Bill*. No credit card required.
*Terms and conditions apply.






