Remembering the MSP guidelines for billing isn’t always easy. It’s common to see rejections, especially when you’re just starting out. However, while many rejections are fixable, receiving them can mean a delay in your pay, or earning less money than you had planned for. There are three main groups of where errors are encountered:
- Data Capture
- Call Out/Continuing Care
- Consults and Visits
Most of these rejections, mistakes, or missed billing opportunities are preventable. Avoiding these common pitfalls early can save you valuable time.
Data Capture
Many of the most common mistakes in MSP billing come from mistakes in capturing or inputting patient data. These kinds of errors are easy to fix, but can be time-consuming if they’re missed - so the best way to handle them is to prevent them from occurring in the first place!
1. Wrong PHN
One common mistake is inputting the incorrect patient health number, or finding out too late that the patient is missing insurance. To prevent this, check with your billing provider to see if they have any automatic data collection tools or insurance eligibility checks. For example, with Dr.Bill, we automatically run eligibility checks on refused claims and resubmit anything that’s eligible.
2. Forgetting a Referring Physician
Unless you’re the first point of contact for a patient, consultations and visits typically require a referring physician. If you don’t add one, your claim will be rejected - so make sure to double check before you submit.
3. Failing to Meet Code Requirements
Some fee codes can only be used when the visit requires a specified amount of your time, such as fifteen minutes. Using the code for a shorter visit goes against the rules, and you’d end up having that claim rejected.
4. Patient Name is Incorrect
Sometimes the name provided by the patient won’t match the information MSP has on file. If this is the case, MSP will let you know the patient details are incorrect and that you will have to fix your submission. If you’re billing with Dr.Bill, our billing agents would handle all patient updates for you.
5. Location of Fee Code Doesn’t Match
If you bill a fee code with the wrong location - like a radiology code in the ER - MSP will catch the mistake and reject your claim.
Call Out/Continuing Care
Billing for call outs and continuing care is one of the most complex aspects of MSP billing. Before getting into the common mistakes, it’s a good idea to understand how call outs and continuing care payments work.
- Call outs are premiums that get added to a claim when you’re called in from outside of the hospital to come care for a patient.
- Continuing care happens after you’ve logged a call out charge and continue to care for patients.
These premiums are meant to incentivize doctors to assist in urgent health situations - and while they can give you additional income, there are more rules associated with them. It’s important to learn how to use them correctly. Here’s what you need to know:
6. Call Outs:
- You can use call out premiums if you’re called out to the hospital on an urgent, non-elective basis, using billing items (01200, 01201, 01202).
- These premiums are based on the time in which you were called. During weekdays, if the call is after 6 pm but before 11 pm you’d bill 01200 for evenings. If the call is after 11 pm but before 8 am you’d bill 01201 for nights and if you were called in over the weekend or on holidays you’d bill 01202.
- If the call is during regular weekday hours, you would bill an emergency visit instead - which includes both the visit and the surcharge for the call.
- You will need to provide 30 minutes of continuous care before using the call out premium - the timing for call outs begins after the first 30 minutes for consultations, visits, or anaesthetic evaluations. Payment is based on one half hour of care, or the major portion of it (at least 15 minutes).
- These premiums can’t be used on routine visits or rounds - if you’re scheduled to be there, you cannot bill for these codes.
7. Continuous Care
- Continuous care premiums are eligible after you provide 45 minutes of continuous care - the initial 30-minute refractory period, plus the 15-minute major portion.
- After this 45 minute period, if you’re still at the hospital and still treating patients, you can then add the continuous care premium to your claims.
- Continuing care surcharges can be used (with codes 01205, 01206, 01207) on top of each half-hour of care that is provided, as long as the criteria for the fees are met (no routine visits or rounds).
- Continuing care premiums should be added to your claim in addition to a note with ‘CCFPP’ (Continuing Care From Previous Patient); this lets MSP know you did not leave the hospital or clinic between patients. If you forget this note, you’ll be deducted 30 minutes from your claim - which, in some cases, is the entire time you spent with the patient. With Dr.Bill, our software will automatically add this note for any claim you toggle continuing care.
- The continuous care premium is based on the total time you spend with the patient, not the number of patients you see - if you see 3 patients in a 30-minute time frame, then you would only add the continuing care premium on the last patient you see, using the entire 30-minute duration.
These premiums work together, so any continuing care premiums won’t be paid until your call out premium is paid - which means that if you have any issues with the call out claim, your claim for subsequent continuing care will also be refused.
Therefore, always double-check your call out claim first - making sure the patient details are correct and that you aren’t missing a referring physician or start/end times. Remember that these premiums are meant for use in urgent or unexpected medical situations where you are called to another hospital to assist - they are not meant to be used on routine rounds or when you’re staying late.
To use these premiums on Dr.Bill, log your consult or visit with the patient, then toggle ‘Call Out’ or ‘Continuing Care’: don’t forget to enter the call time, start time, and end time for the visit. Our software will automatically apply the correct premiums. Only use the ‘Call-Out’ toggle for your first patient. For subsequent claims, just toggle ‘Cont.Care’.
The most common mistakes with these premiums are forgetting to include ‘CCFPP’ in your notes, logging continuing care fees without a call out, and using the continuing care fees when you’re staying late but haven’t actually been called in.
Consults & Visits
Billing for consultations and visits can get complicated, thanks to the different rules and regulations associated with each fee code. However, most of the common rejections come from the same errors:
8. Logging 3+ Directive Care Codes in a Week
A minimum of 2 direct care codes can be claimed per patient per week - adding more than this will end up getting your claim rejected.
9. No Note for Multiple Visits on the Same Day/Duplicate Claims
Duplicate claims aren’t allowed, so make sure that if you’re billing for a consultation with multiple visits, you add the times of the consults and the visits. This is not something you’ll need to do when the visits are billed independently, however, when billed together you will need to include it - this way, MSP knows that the visits occurred at different times, and aren’t just duplicate claims.
10. Incorrectly Billing Hospital vs. Directive Care
Directive care visits are visits from a consultant. Used correctly, they indicate that you are not the most responsible physician and have been called in for your expertise. These visits are worth more than hospital visits, but they can only be billed twice per week - hospital visits (like the ones you would do on your rounds) can be billed daily.
Keep in mind that you can bill hospital daily visits or directive care visits - but not both. Sometimes doctors will choose to bill for hospital visits instead of directive care codes when they expect to see the patient enough times in a week to make it worthwhile to do so. This is allowed; however, sometimes physicians will bill their two directive care visits and then try to claim hospital daily visits afterwards. This is incorrect, and your hospital claims will be rejected.
11. Using Out of Office Premiums on Emergency Visits
When you bill for an emergency visit, your call out and continuing care premiums are included in the fee. By billing them on top of these visits, you’re essentially billing these fees twice - and your claim will be rejected.
12. Same-Day Visits and Procedures
Billing for a visit on the same day as a procedure is allowed, but the visits should have a different diagnostic code from the procedure if possible. If these two items have the same diagnostic code, the lesser fee code will be reduced to 50%.
Although billing can seem daunting at first, it’s important to fix mistakes so you’re paid for all your hard work. Getting into the habit of double checking your claim details and reviewing the rules and regulations set out by MSP, can go a long way in preventing rejections.
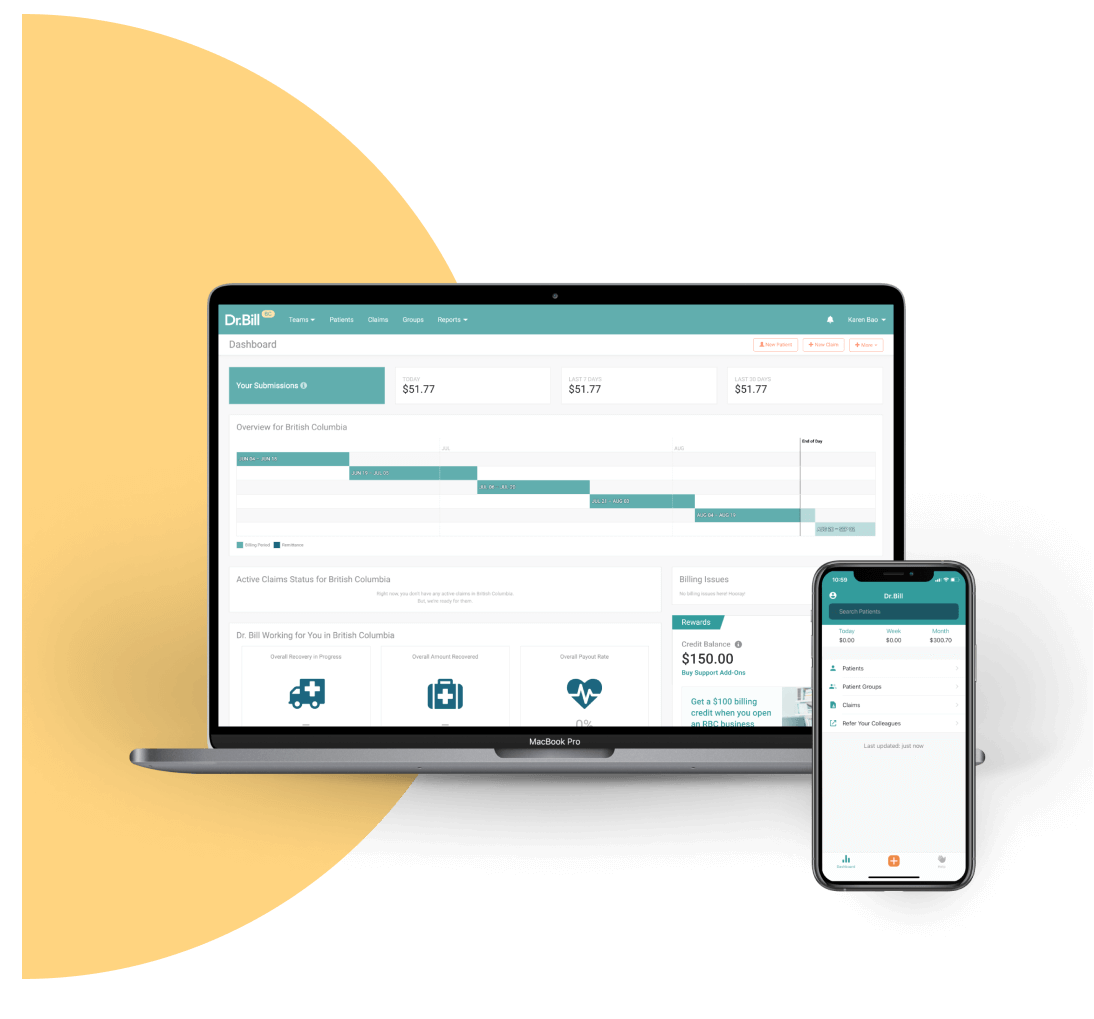
An MSP Expert in your Pocket
Find codes and bill premiums with a tap. Get a $150 Credit when you sign up for Dr.Bill*.






