Whether you’re a plastic surgeon or an epidemiologist, being a doctor in Canada means billing for your time! From using OHIP’s schedule of benefits to filling out worker’s compensation claims, there are a number of ways to bill when you’re practicing in Ontario. Here are the basics:
OHIP Billing
In Ontario, under the fee-for-service model, you’ll be paid by the Ontario Health Insurance Plan (OHIP) per procedure. OHIP has a list of approved procedures that they’ll pay you for. In order to get paid for these procedures you need to submit a claim detailing what the procedure was, who the patient is and where it took place.
In order to submit claims to OHIP electronically you need to have an OHIP billing number and set up OPS BPS Secure (formerly Go Secure), Enrol in MC EDT & Assign a Designee (If you don’t have one yet follow along with these screenshots to set everything up at the same time).
All of OHIP’s approved procedures are outlined in the OHIP schedule of benefits, which is a complete listing of the medical services you can bill for in Ontario. These services – as well as the rules for when and how you can use them – will differ by specialty, so it’s important to know what billing codes are available to you.
With over 6000 services available to choose from, this document is lengthy, but learning more about the billing codes in your specialty can help you to optimize the amount you bill – and ultimately earn. An easier way to find the code you need is to search the Ontario Schedule of Medical Benefits electronically through our OHIP searchable database.
OHIP Fee Code Breakdown
The first digit of the code tells the government what kind of patient you are seeing. For example, in the fee code A005a, the ‘A’ means the patient is an outpatient. If the code began with the letter ‘C’, the patient would be an inpatient, and if it started with an ‘S’, it would refer to a surgical procedure.
The next two digits represent the type of doctor performing the work. In the example of A005a, ‘00’ represents a family physician – ‘13’ would refer to an internal medicine specialist, ‘60’ would be a cardiologist, and ‘03’ would be a surgeon. The third digit of the fee code describes the service provided. In this example, the ‘5’ in A005a would refer to a consultation, but a ‘3’ would tell you it is a special assessment. Codes for all specialties can be found in the schedule of benefits.
Lastly, the suffix refers to your role in the services performed. If you’re the consulting physician or surgeon, you would use the letter ‘A’. If you are assisting (for example, in a surgical procedure) you would use the letter ‘B’, and if you are the anesthesiologist in a surgical procedure, you would use a ‘C’.
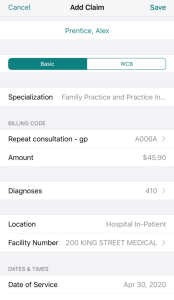
OHIP Required Billing Information
In addition to using the required OHIP fee codes for the services you bill, you’ll also need to ensure your OHIP claims include the following information:
- The patient’s name
- A billing code
- Up to 3 diagnoses (ICD9s)
- A service location
- A facility
- The date of service
- The start and end times
- A referring physician
When your claim is completed, it should look like this:
If you make a mistake then OHIP will refuse or reject to pay your claim.
What’s the difference between a refusal and a rejection?
A refusal means your claim has a simple error (one that you can fix and resubmit quickly like a mistake in your patient’s name or you forgot to add a referring physician). A rejected claim means your claim has ‘gone against’ a billing rule – these take longer to fix and aren’t guaranteed approval. Handling refusals and rejections tends to be time-consuming. When you’re looking for a software system to submit your OHIP claims, always choose one with rejection management (like Dr.Bill of course)!
Other Types of Billing
Billing through OHIP will likely make up the majority of your income. However, there are other types of billing that you may need to do which aren’t directly covered by OHIP. To make sure you get paid for every patient you see, you’ll need to make sure you know how to bill properly in these situations as well:
Out of Province
When seeing out of province patients, who don’t have OHIP coverage but do have coverage through their home province, you can still bill OHIP thanks to the reciprocal payment program – in which all Provinces and Territories, except Quebec, have agreed to pay for insured services provided to residents of other provinces when a patient presents with a valid Provincial Health Registration Card.
Just make sure you have the correct billing address and health care number and submit the claim like you normally would to OHIP.
Quebec
Patients in Quebec cannot be billed through the reciprocal program – for these patients, you’ll need to send an invoice to the provincial health body or directly to the patient. The patient will then be reimbursed by their insurance provider.
Uninsured Patients
Even if the patients you treat do not have insurance – for example, if they live outside of the country, or live in Quebec – you will still be able to get paid through private invoicing.
You can use Dr.Bill’s private invoice template to send private invoices directly to your patient.
**This is a feature only available on the web app (not mobile).
To generate a private invoice simply:
- click on “New Patient”
- toggle the patients profile to “Private”.
- enter all of their details and click “Create and Start a Claim”
- after you finish entering the claim details click on “Create Private Invoice”
- enter in invoice details and click on ‘create invoice’ to print/save off the invoice and send it to your patient.
Follow along with detailed photos of how to use our templates to bill your uninsured patient directly:
Private Invoice Templates
WSIB Claims
To treat patients who have been hurt at work, you’ll need to register with the Workplace Safety and Insurance Board (WSIB).
How do I bill when I treat an injured/ill worker?
When you treat someone who has been hurt at work, you’ll be paid for both the insured services you provide and for the reports you’ll need to make for WSIB. Unfortunately, to get paid for both the service and the reports you’ll need to submit 2 separate claims through two separate services. Here’s how:
-
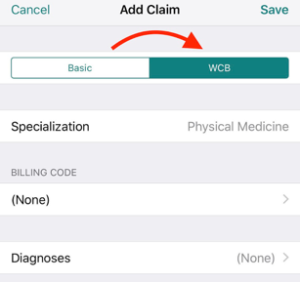
WSIB Insured Services
For insurable medical services, you’ll submit a claim to OHIP the same way you normally would – the only difference is you’ll need to indicate “WCB” on the claim instead of basic. OHIP will pay you for your time and bill WSIB themselves.
When you’re using Dr.Bill, this means selecting ‘WCB’ instead of ‘basic’ on the top of your claim submission, like this:
-
WSIB Reports
When you treat a patient who has been injured at work you’ll also need to fill out a form in addition to submitting a claim. This form details what happened, what you did and the state of your patient. WSIB pays you for the forms you fill out, but you’ll need to invoice them directly. You can do this through the online Telus Health portal. Keep in mind that these claims will use a different set of fee codes from OHIP, which will let you know which form/code to use. You can find these on the WCIB Physician Fee Schedule.
How to register:
To submit your WCIB forms to Telus Health, you’ll need to follow the online instructions and register with the WCIB on Telus Health. Keep in mind that whether you’re submitting your WCIB claims for services through OHIP or submitting your forms to their online portal, you’ll need to register first.
RCMP/DND/Refugees/Prisoners
RCMP officers, DNDs, refugees, or prisoners should be invoiced privately. Each of these categories has a specific identifier, and you’ll need to add this number to the patient card. For example, if you are using Dr.Bill and see a prisoner, you can add them using the 7-9 digit correctional ID or CS number given by the prison. Since you might not see these types of patients as often, it’s a good idea to double check the information you’ll need with your billing software to make sure you have everything in place.
Conclusion
Billing for your time is easier than you think! Once you’ve gone over the approved services in your specialty and have gotten the hang of what fee codes are available to use, it ‘almost’ becomes second nature. To really make sure you don’t get penalized for any errors you make just remember to use a billing provider with rejection management.
This article offers general information only and is not intended as legal, financial or other professional advice. A professional advisor should be consulted regarding your specific situation. While information presented is believed to be factual and current, its accuracy is not guaranteed and it should not be regarded as a complete analysis of the subjects discussed. All expressions of opinion reflect the judgment of the author(s) as of the date of publication and are subject to change. No endorsement of any third parties or their advice, opinions, information, products or services is expressly given or implied by RBC Ventures Inc. or its affiliates.