Working as a doctor in BC means that sometimes you might treat a patient who has been injured at work. Workplace injuries are claimed electronically through teleplan – which means you can submit them directly through your billing software. However, instead of your claims being sent to BC’s Medical Service Plan (MSP) they go to ‘The Workers’ Compensation Board of British Columbia’ (WSBC). WSBC claims are often referred to as WCB claims as the national legislation is known as the Workers Compensation Act.
Most of the routine medical services, such a regular office visits, are billed to WSBC using MSP codes, however, there are some fee codes and reports that are unique to WorkSafeBC. This mini-guide will walk you through the general WCB claim process and show you how to submit the various WorkSafe BC physician codes and forms.
1. Register for WorkSafeBC Physicians
There’s no formal process or contract required to work with WSBC but you should check with your billing service to see how to submit WSBC claims, as it varies depending on the software. If your software program doesn’t provide it you might need to create an account directly with WSBC.
2. How to Submit WSBC Claims
The following instructions are specific to Dr.Bill, which means the exact process may differ depending on who you’re billing with, however it should be somewhat similar. That being said, we’ve worked hard to streamline the process and make it as simple as possible.
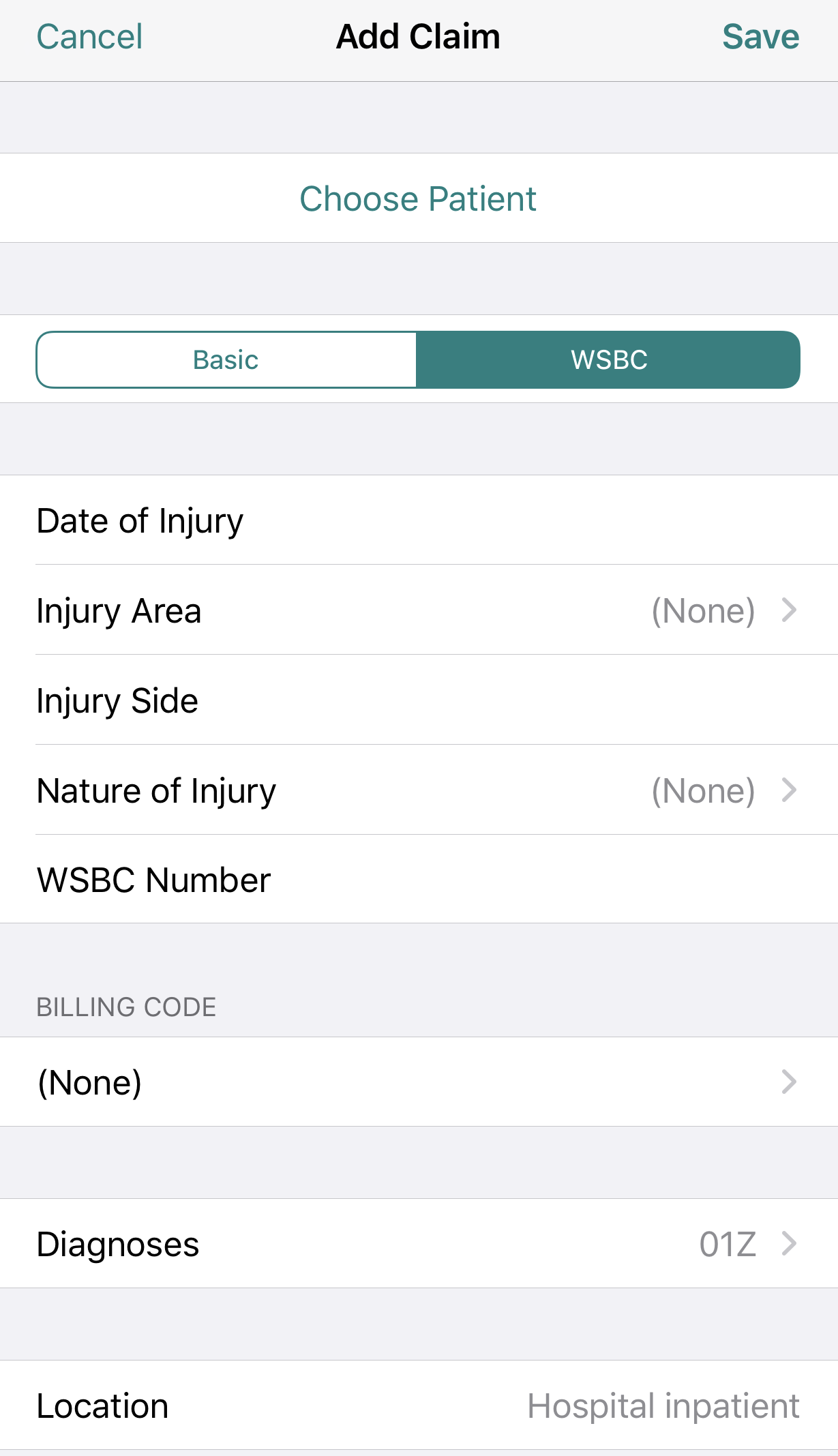
Create a WSBC Claim
- Add your new patient or pull up an existing one.
- Select WSBC instead of ‘basic.’ This changes the menu to reflect the relevant WSBC fields:
- Date of injury
- Injury Area
- Injury Side
- Nature of injury
- WSBC claim number (if known
- Create a new claim and enter the details as you would normally.
Once you complete all the fields click save to submit it to WSBC through teleplan.
Medical billing in BC is confusing and can often be overwhelming. To help out, check out our complete MSP guide that walks you through each step of medical billing – from the general teleplan process to maximizing your claims and using mobile billing.”
3. How to Submit WorkSafeBC Physician’s Report (form 8/11)
Sometimes you might need to send a report to WorkSafeBC if you suspect that your patient will be disabled beyond the day of the injury or if the claim is for one of the following:
- a hernia
- back condition
- shoulder or knee strain/sprain
- occupational disease, or
- mental disorder.
You need to send this report within 3 business days of the patient’s first visit. There are two types of forms. The first is form 8, the ‘first report’ form, which you’ll fill out when you believe that your patient will be injured for longer than 1 day.
The second is form 11, the ‘condition or treatment change’, where you’d outline any changes in your patient’s treatment or condition since the last report. You also need to fill out form 11 when your patient is ready to return to work.
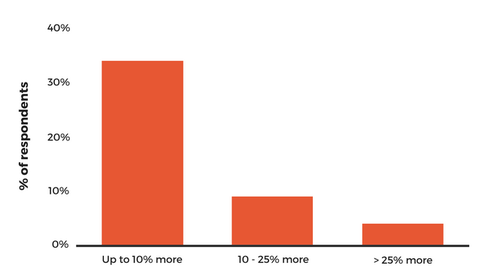
Both Form 8 and 11 are time-sensitive paid, meaning you might be paid less depending on the date that WorkSafe BC receives the completed application.
Form 8 and Form 11:
- received 0-3 days paid in full
- received 3-6 days paid at discount
- received 6+ days paid at zero
Fee Codes that need form 8:
19937 WorkSafeBC Teleplan E-Form 8 Received Within 3-6 Days.
19900 WorkSafeBC First Report Of Injury (Form 8) Received Within 3-6 Days – Fax.
19927 WorkSafeBC First Report Of Injury (Form 8) Requested, Received within 10 Days.
Fee Codes that need form 11:
19940 WorkSafeBC Teleplan E-Form 11 Received Within 3 Days.
19902 WorkSafeBC Progress Report (Form 11) Received Within 3-6 Days – Fax.
For a list of all WorkSafeBC unique fee codes use our searchable database:
If you believe your patient will be hurt longer than one day it’s best to fill out form 8/11 on the same day you submit your claim. When you’re submitting a 8/11 forms make sure you have the criteria needed below in order to reduce the chances of forgetting something. This is the same criteria you needed to include in your WSBC claim sent through teleplan:
- AOI – area of injury
- NOI – nature of injury
- DOI – date of injury
- Location: – Right, Left, neither or both
- WSBC claim number – if known
Billing Tip: Any overlapping information on your WSBC claim and WSBC forms must match otherwise your claim will be refused.
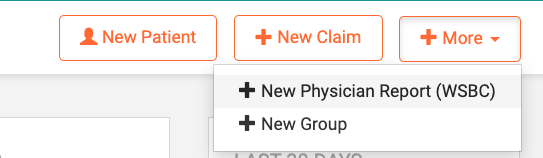
You can fill out form 8/11 on the web version of Dr.Bill by following these instructions:
- Sign in on the web browser
- On the right-hand side of the screen click on ‘+more’ then on the drop-down menu choose ‘New Physician Report WSBC’
- Completed and fill out the form with the following details:Patient: enter your patient’s name. WorkSafeBC claim number: (leave blank if you don’t know it). Service Location: where was it done, example “E” for ERDate of Service: date the assessment was doneDate of Injury: date when the injury occurred. If it’s an occupational disease, choose the date when medical attention was first requested.
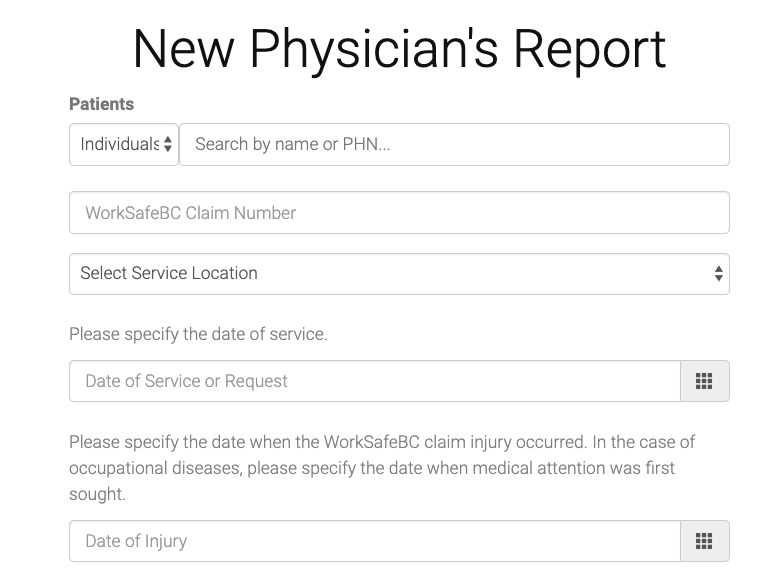
- Next, this is where you choose between form 8 (first report) or form 11 (Condition or Treatment Changed).
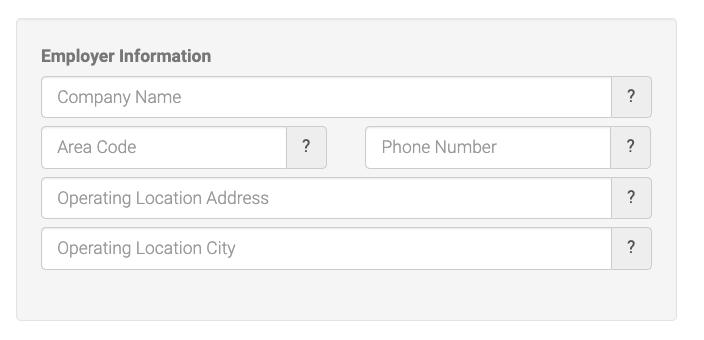
- Fill out your patient’s employment information.TIP: Often patients can be reluctant to provide full details of their employment, in hopes to avoid workplace conflict. Try to get at least the company name and a phone number. Then, if you need to, you can google the rest.
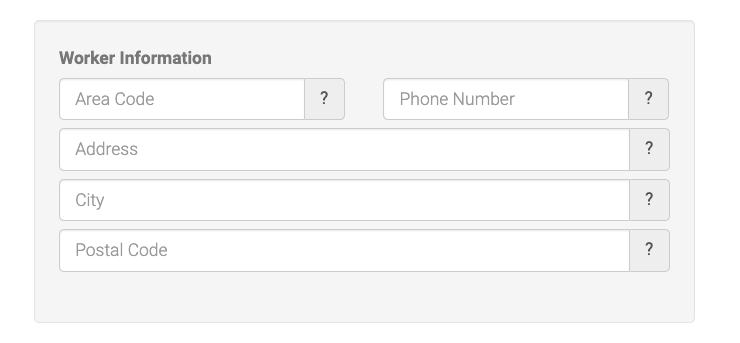
- Fill out your patient’s information.If your patient is unresponsive or unable to provide these details, it’s best to put “unknown” as opposed to leaving anything blank, which may cause the claim to get rejected.
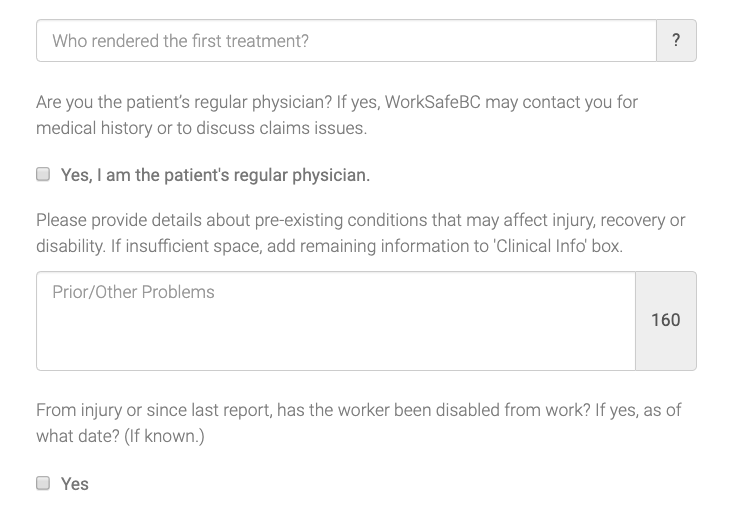
- For the next section fill out who was the first person to treat the patient. Examples; Medic, First responder, ER physician (but not the first-aid at the worksite).TIP: Don’t leave any boxes empty or it’s often considered incomplete. For example, where it says ‘Prior/other problems’ write “NONE” if the patient doesn’t have any pre-existing conditions.
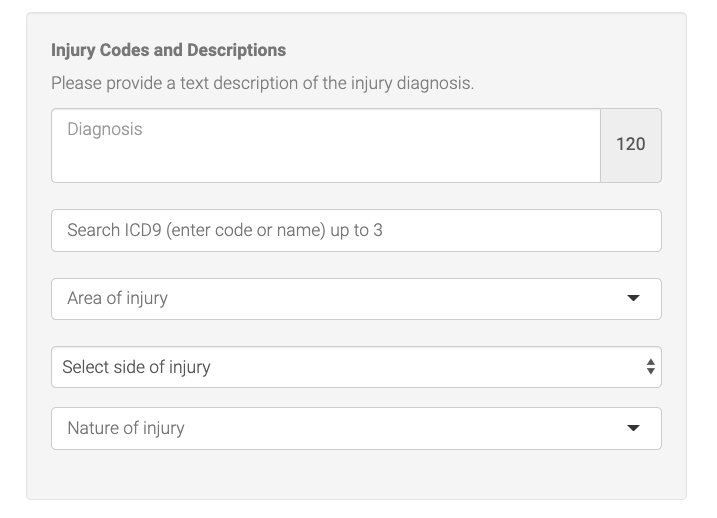
- The next section is where you’ll enter the injury details:TIPS:
- Diagnosis: can also be ICD 9 code but best to use full written diagnosis.
- ICD 9 code: you can select up to 3.
- Area of Injury: body part – such as Scalp, Leg, Arm etc.
- Side: Right, Left, neither or both
- Nature of injury: Strain, Fracture, Laceration etc.
- Clinical information: document your findings from the assessment.
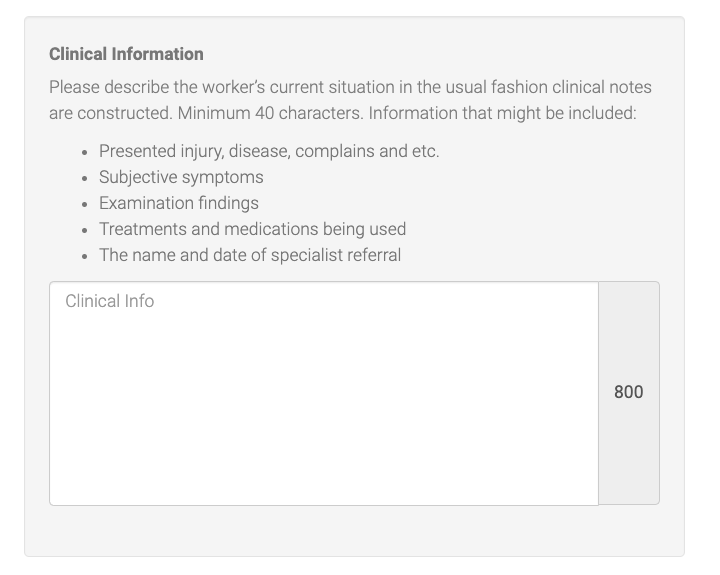
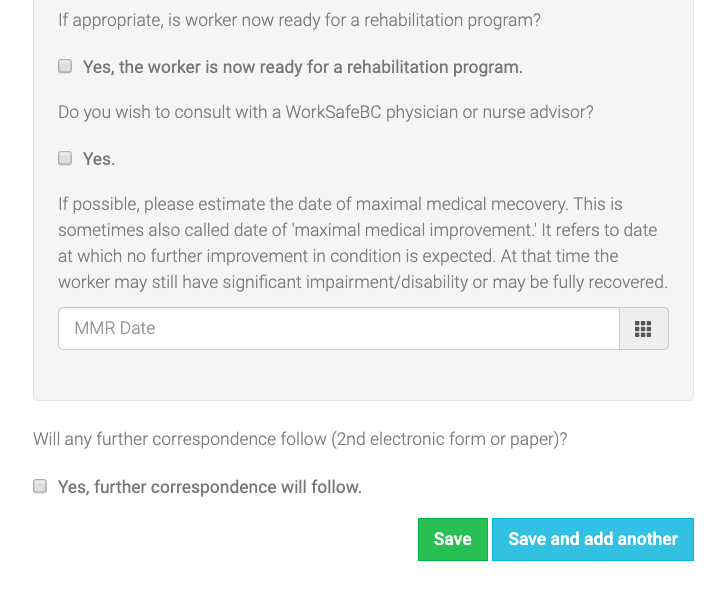
Return-to-work: Fill out when you think your patient will be able to return to work. There’s a space where you can select an estimated amount of time (days, weeks, months).
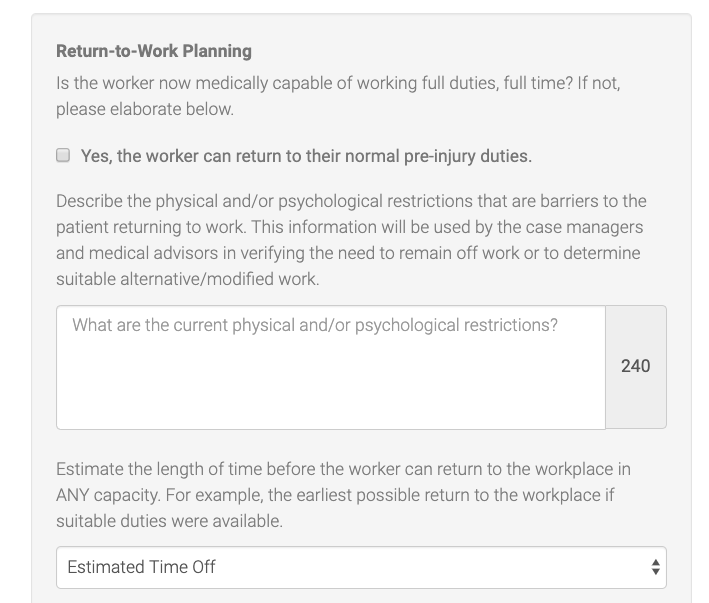
TIP: Be sure to toggle all buttons and complete all boxes. For example, if the patient is returning to work with no restrictions – simply put “RTW -no restrictions” in the box provided above. If anything’s left blank it might result in a rejection.
- Save and you are done!
All 3 reports below need to match, otherwise except delays and/or rejections.
- Physicians reports
- Employer report
- Patient report
4. How to Submit WSBC out of province/uninsured claims
WorksafeBC typically only insure claims for BC residents who have valid insurance.
However, if your patient has insurance from outside of BC or doesn’t have insurance at all, but has a valid WorkSafeBC claim, you can still submit it electronically to WorkSafeBC using generic patient data. WSBC created this data specifically for out of province or uninsured patients.
Here’s the patient data you’d need to enter for out of province or uninsured WCB patients:
- Patient: WCB, Hospital
- USE PHN: 9152 416 049
- DOB: Dec 2, 2002
- Last Name: WCB
- First name: hospital claims
Remember to click on WSBC instead of MSP and fill out all of the fields.
At the bottom of your claim you need to include the following information in a mandatory note:
- Your patient’s full name
- Date of Birth
- Alternative provincial health care number (if your patient doesn’t have insurance write uninsured).
Example: Smith, John – 07jul1992 – ON PHN 012000.
5. WSBC Expedited Consultations
You can bill an initial or repeat expedited consultation if you’re a specialist physician or a referring physician. If you’re a non-specialist physician with areas of expertise (for example, sports medicine) then you need to get pre-approval by WSBC beforehand. If that’s the case call 1-604-276-3344 (or 1-888-967-5377 ext. 3344).
An expedited consultation includes both the physical examination and the report. This means you won’t be able to use any other office visit fee codes or report fee codes in addition to this.
Your report needs to contain the following information:
- Purpose of examination
- Nature of injury
- Your patient’s present complaints
- Objective findings
- Diagnosis or differential diagnosis
- Information regarding causation including risk factors other than work; and
- Recommendations regarding work restrictions as related to the work injury/disease.
WSBC needs to receive the report within 15 days from the referral.
For any other Consultations (e.g. Repeat Consultation scheduled by the consulting physician versus being referred): the report must be received within 5 business days of the consultation.
If you’re the consulting physician and you believe that your patient is able to return to work then the report needs to be received within 3 days of the consultation.
Billing Tip: If you go over the time frames above, then bill an MSP consultation fee code for your specialty. And, (if applicable) bill 19908 (a non-expedited specialist consultation report) for consultation services that do not include a report in the MSP fee item description. You can use 19908 for an initial or repeat consultation but WSBC needs to receive it within 7 days of DOS.
Initial and Repeat Expedited Comprehensive Consultation Guidelines:
- The initial consultation is used only for the first time you see someone or if it’s been 6 months since you last saw them. You’re also allowed to bill it if you’ve seen the patient before but this time it’s under a new referral.
- You can bill a repeated consultation when it occurs within 12 days of the first consultation – anything else won’t be eligible for payment.
Billing TIPS: If you’re giving a post-operative consultation then bill the follow-up visit and report as 19931 (the post-operative consultation). It’s not considered a repeat consultation and WSBC won’t reimburse you for it.
6. WSBC Expedited Surgery
Before surgery, you need authorization from WSBC, which you can get by filling out form 83D6 (Authorization Request for Surgery) within 5 business days of the Consultation Report that includes the recommendation for surgery. Print the report and fax to WSBC to (604) 233-9777 or Toll-Free at 1 888 922-8807.
Once you get approved for surgery it must be done within 20 business days from the last consultation. If it’s done after 20 days then it won’t be eligible for payment – at which point you can bill it under a regular MSP fee code.
The only exception to this is if you’re performing Extensive Spine Surgery (which requires multilevel procedures or revisions), and therefore the 20-day limit doesn’t apply.
After the surgery, you’re required to fill out an operative report, which WSBC needs within 20 days from the date of surgery.
WCB Reminder: Getting authorization for surgery doesn’t mean you’ll be paid expedited rates. Only the first 3 elective surgeries (per patient) are eligible for expedited payment. This applies only to repeat surgeries performed on the same site.
If your patient needs an additional surgery then you’ll need to get a second opinion by a Richmond VSC Specialist and further surgery will require authorization from the Health Care Services Program Manager. If that’s the case call 1-604-276-3344 (or 1-888-967-5377 ext. 33
44) and WSBC can provide you with the exact steps depending on your situation.
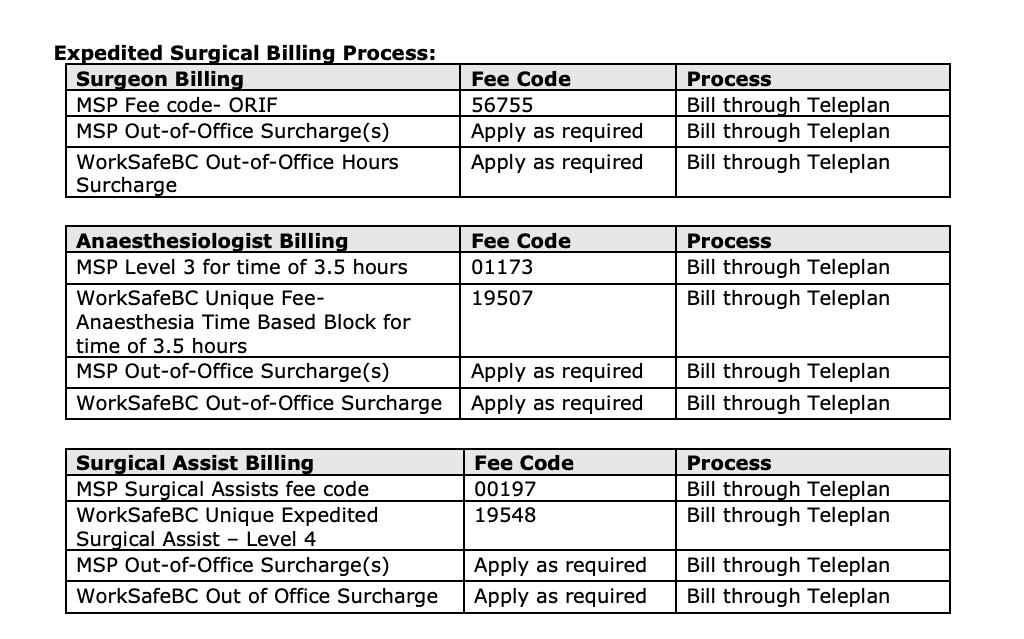
7. How to Bill WSBC for Expedited Surgery
- Bill the applicable MSP Surgical Procedure Fee Code and fill out the claim with the necessary information (toggle any MSP premiums like call-out/cont.care if applicable).
- Click save, then, if you qualify for WorkSafeBC out-of-office surcharge create a second claim for:
- Fax the operative report to (604) 233-9777 or Toll-Free at 1 888 922-8807.
8. How to Bill WSBC for Surgical Assistants
- Bill the applicable MSP surgical assist code. Remember surgical codes are percentage-based fee codes based on the value of the surgery: 00195 Surgical Assist less than $317 Inclusive
00196 Surgical Assist $317 to $529 Inclusive
00197 Surgical Assistance – Operations over $529Then, fill out the claim with the necessary information (toggle call-out/cont.care if applicable) and click save. - Fax the operative report to (604) 233-9777 or Toll-Free at 1 888 922-8807
9. How to bill WSBC for Anesthesia Surgical Services
- Bill the applicable MSP fee code (Intensity/Complexity Levels). Fill out the claim with the necessary information and click save.
- Bill the unique WSBC Fee Code 19507 (Expedited Anesthesia Services). This is a time-based fee code per a 15-minute time block.
- A copy of the Record of Anesthesia must be faxed to (604) 233-9777 or Toll-Free at 1 888 922- 8807. Be sure to include the Claim Number on the Record of Anesthesia (otherwise it will come back as rejected).
The anesthetic time includes a pre-operative assessment, as well as the time from inductions, until your no longer in attendance and the patient is safely discharged for the post-anesthetic recovery (PAR).
If the pre-operative and PAR times are significantly longer than 15 minutes, or a total of thirty 30 minutes, then you need to add an explanatory note at the bottom of your claim to briefly explain why.
10. WorkSafeBC Expedited Surgery Billing Example
Here’s a billing example of an expedited surgery directly from WSBC:
- Surgery: Fractured Tibia- Open Reduction & Internal Fixation (ORIF)
- Time: Tuesday 0125-0425 hours
- Surgery duration: three (3) hours
11. WSBC Explanation Codes
If you submit a claim and it doesn’t pass the approval process then it may be rejected, reduced or refused.
When this happens you’ll be given an explanatory code for why each rejection, reduction or refusal happened. To find out what that code means find a description below (WCB and MSP codes are all listed):
If you have any questions about WorkSafeBC claims or would simply like to clarify something, don’t hesitate to get in touch with us.