Working In Obstetrics can be exciting, rewarding and sometimes emotionally demanding.
At the end of a long day you want to be able to bill properly for everything you did, without worrying if your claims are going to come back rejected. Knowing which billing fee codes are available within your specialty is a great way to maximize your claims while reducing your chances of getting rejections.
In an effort to save you time, and headaches, we’ve put together a quick reference of MSP billing tips for Obstetrics practitioners.
Don’t forget to bookmark it, or for a printable PDF that you can hang up in your workspace scroll to the bottom.
MSP billing tips for Obstetrics practitioners
Called from outside the hospital:
Only one call back is typically paid unless you can provide an exceptional reason for the extra call back. If you do try to bill more than one, you need to leave a note In the MSP note field explaining why.
00112 (0800-1759) Weekdays – Includes the visit fee
01200 (1800-2259)
01201 (2300-0759)
01202 (0800-1759) Weekends and Stat Holidays
QUICK TIP:
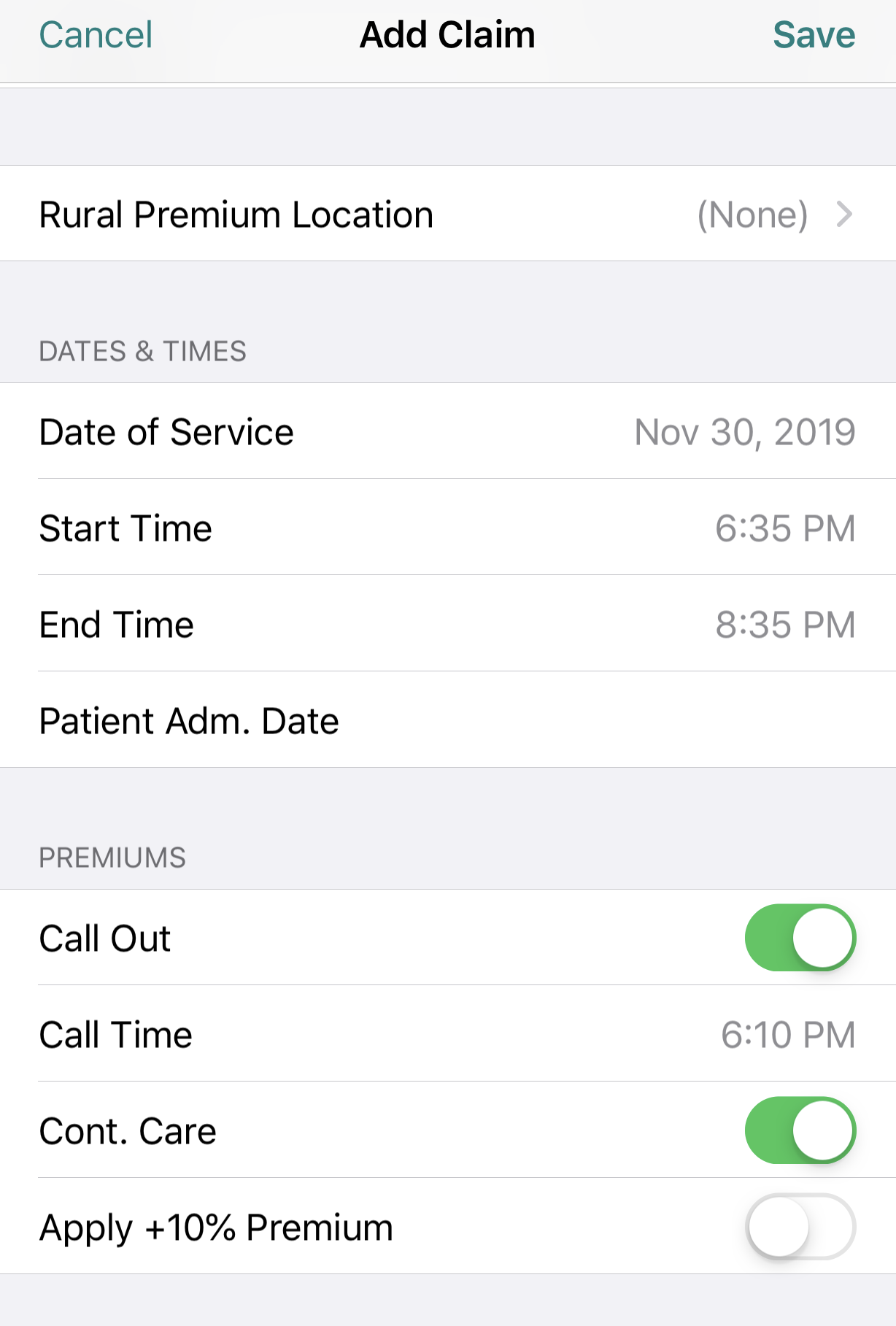
If you’re using the Dr.Bill app, log the claim like you normally would then, at the bottom of the claim toggle ‘Call Out.’ Don’t forget to enter the ‘Call Time’, ‘Start Time’ & ‘End Time’ for your encounter. Our mobile app will automatically apply the correct Out of Office premiums to your claim.
If you’ve logged a Call Out charge and then continue to see additional patients you would be entitled to bill continuing care surcharges for each 30 minutes after the initial 30 minutes you spent with the patient you were initially called to see.
If you’re billing continuing care during a delivery it’s only eligible from the start of the 2nd stage. You need to leave a note In the MSP note field saying ‘‘2nd stage started at 0000 to delivery of baby at 0000.’
To apply this premium toggle both ‘Call Out & Continuing Care’. Like this:
Called from inside the hospital:
The same rules apply as above; typically only one call back is paid unless you can provide an exceptional reason for the extra call back. If you do try to bill more than one, you need to leave a note In the MSP note field explaining why.
00113 (1800-2259)
00105 (2300-0759)
00123 (0800-1759) Weekends and Stat Holidays
Assessment Fee (13200):
Billed in addition to a call out fee, if no delivery fee is billed. If the delivery occurs later that day, you need to add a note with the assessment stating the patient was not in labour.
Delivery Obstetrics Fee Codes:
14104 Vaginal Delivery
14105 Management of Labour and Transfer to Higher Level of Care Facility for Delivery.
14108 Elective C/S – ADD SURGICAL ASSIST 00196.
14109 Emergency C/S – ADD SURGICAL ASSIST 00196 (May also qualify for surgical surcharge).
BONUSES for Obstetrics Practitioners:
Maximum of 25 total for the calendar year:
Medical billing in BC is confusing and can often be overwhelming. To help out, check out our complete MSP guide that walks you through each step of medical billing – from the general teleplan process to maximizing your claims and using mobile billing.
Obstetrics Fee Codes for Complicated Deliveries:
These fees are the same for OB and only one of you can bill them. Discuss with the OB if you request a consult to see who will bill these items if applicable.
04000 Complicated Delivery
04014 Forceps Delivery
04018 Vaginal Breech Delivery
04022 Repair of 3rd degree tear
04023 Repair extensive cerv./vag. laceration
04024 Repair of 4th degree tear
04026 Manual removal of retained placenta
Surgical Assist Obstetrics Fee Codes:
00196 Surgical Assist – Operative Fee $314-523
00197 Surgical Assist – Operative Fee over $523
13194 First Surgical Assist of the day (GP only)
Surgical Surcharges:
01210 (1800-2259) – 44.46% of Surgical Assist Fee
01211 (2300-0800) – 71.37% of Surgical Assist Fee
01212 (0800-1759) Weekends and Stat Holidays – 44.46 % of Surgical Assist Fee
Prolonged 2nd Stage:
A note is required stating the ‘Time Fully Dilated,’ and the ‘Delivery time,’ as well as 2nd stage prolonged. After 2 hours, 14199 is billable each half hour.
The Start time should be the start of 2nd stage, after you have deducted 2 hours.
Continuing Care Surcharges:
Only billable during 2nd stage and after 30 minutes. A note is required stating ‘Time Fully Dilated’ and ‘Time Delivered.’ Billable every additional 30 minutes or major portion thereof.
01205 (1800-2259)
01206 (2300-0759)
01207 (0800-1759) Weekends and Stat Holidays
Oxytocin:
Continuous attendance or immediate availability required.
04118 First Hour (times must reflect first hour)
04119 Subsequent hours to a maximum of 10 hours (Start time should be start of the second hour).
Prostaglandin Gel or Cervidil:
Only billable as a visit fee (00108 or 13200), unless it is the only fee item billed that day. A call out charge would then be billable with the visit and an electronic note stating “Prostaglandin gel/cervidil inserted”.
13200 Outpatient
00108 Inpatient with 13108 1st Inpatient seen.
Miscellaneous Obstetrics Fee Codes
00199 You could bill this for attendance during weekday hours for example with postpartum hemorrhage, or fetal compromise before start of second stage.
You need to leave a detailed note In the MSP note field and a billed amount that seems fair and explainable.
04699 Examination of Ferning (Only billable with Outpatient Location Code)
MSP billing tips for Obstetrics practitioners
If you’re interested in other MSP fee codes, make sure to save a link to our MSP searchable database below. You can search by specialty, billing code or keyword.
MSP billing codes Searchable Database
Explanatory Codes
If you do submit a claim and it doesn’t pass the approval process by MSP your claims may be rejected, reduced or refused. This can happen for a variety of different reasons (around 706 different reasons to be exact)!
In our experience, these are the most common scenarios to watch out for:
- Location of fee code doesn’t match. Ie, radiologic fee code performed in ER
- There’s a fee code conflict – so assessment is required
- Invalid use of Premiums
- No Referring Physician
- Patient doesn’t have insurance
Extra Reminder: A lot of errors are a direct result of either not adding a referring physician OR not double checking that your patient has insurance. Always make sure you check these two things before submitting your claim.
If you’re patient doesn’t have insurance, don’t worry, you can still get paid if you submit a private invoice. It’s the same as submitting a claim to MSP only you select private instead of public.
If you do make a mistake, you’ll be given an explanatory code for why each rejection, reduction or refusal happened. To find out what the code means, find the description below:
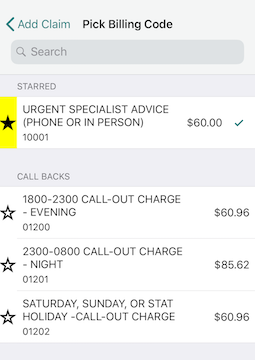
Starring
Remember you have the option of ” starring” your most commonly used billing codes. That way, they’ll appear at the top of your list for easy-searching.
If you found this useful, or would like to see more MSP billing tips, let us know on twitter.
This article offers general information only and is not intended as legal, financial or other professional advice. A professional advisor should be consulted regarding your specific situation. While information presented is believed to be factual and current, its accuracy is not guaranteed and it should not be regarded as a complete analysis of the subjects discussed. All expressions of opinion reflect the judgment of the author(s) as of the date of publication and are subject to change. No endorsement of any third parties or their advice, opinions, information, products or services is expressly given or implied by RBC Ventures Inc. or its affiliates.






