Effective May 1, 2020, any pending COVID-19 K-codes can be submitted to OHIP for reimbursement. This includes the temporary fee schedule codes ( K080A, K081A, K082A, K083A) along with the sessional fee schedule code H410A.
Note: For any claims created on Dr.Bill that were pending, we will automatically submit them for you and adjust any changes they may need.
For a summary from the original OHIP bulletin of COVID-19 guidelines and changes please see below:
Fee for Service Claim Submissions Guidelines:
- Eligible payment programs to submit claims for K080A, K081A and K082A include Health Claims Payment program (HCP), Workplace Safety and Insurance Board (WCB) and Reciprocal Medical Billing (RMB) where the billing number is in the range of 010009 to 333798.If a you submit a claim with a billing number outside this range the claim will reject “V35-Invalid OOP/OOC Service.”
- K080A-K083A require a diagnostic code to be submitted on the claim. If claim is submitted without a diagnostic code the claim will reject “V21-Diagnostic Code Required.”
- If a claim is submitted that exceeds the maximum number of services allowable for the temporary fee codes, the claim will reject “A3H-maximum number services FSM.”
- If a claim is submitted under an Assessment Centre group number for these new K codes, the claim will reject “ESF-Not eligible to bill FSC.”
- K080A-K082A will pay $0 with explanatory code “D7-Not allowed in addition to other procedure” when K083A has been previously paid or is on the same claim for same physican, patient and service date.
- K083A can only be billed by specialists. If claim is submitted for K083A by physician with specialty code ‘00’ the claim will reject “A3F-No Fee for Service code.”
- If a claim for K080A-K082A has already been paid or appears on the same claim for same physician, patient and service date and a claim is submitted for K083A, the claim will pay at $0 with explanatory code “D7-Not allowed in addition to other procedure.”
- All new fee codes are excluded from telemedicine. If a claim is submitted with an SLI code ‘OTN’, the claim will reject “TM3-Service not payable under telemedicine”.
- For K083A the fee will be set at $5.00 and the physician should submit the number of services necessary to make payment equivalent to a service provided, rounded to the nearest $5.00.
- For Fee Schedule Codes using time units, calculate units by taking the normal fee and rounding it to the nearest $5, then divide that number by 5. For example, K197 (2 units or 46 minutes minimum) is $173.70 ($86.85 per unit). Now round that number to the nearest $5 ($175) and then divide by 5 = 35 units. You should submit this number as the number of services on the claim and a fee billed of $175.
- For Fee Schedule Codes not based on time units round to the nearest $5 and divide by 5. For example, an A485 consultation is $170.10. This rounds to $170 or 34 units. This code would be billed at $170 with the number of services equal to 34.
- K083A when billed by a Primary Care affiliated physician who has a non-‘00’ specialty and who bills with that specialty will pay FFS and the service will not accumulate to any caps or ceilings
Assessment Centres Fee Schedule Codes H409A and H410A Guidelines:
- H409A and H410A must be billed with the unique group number assigned to each individual Assessment Centre.
- Claims submitted for FSCs H409A and H410A are only eligible for payment if submitted with payment type HCP.
- Claims submitted for Fee Schedule Codes H409A and H410A must be billed with a blank health number (no zeroes or spaces in that field). If not the claim will reject “VHBNo HN Required for FSC.”
- Claims submitted for Fee Schedule Codes H409A and H410A must be billed with a blank version code and blank date of birth.
- H409A is for services provided Monday to Friday 7am to 5pm and is not payable on weekends and statutory holidays.
- H410A is for services provided Monday to Friday 5pm to 7am and all day on weekends and statutory holidays.
- If a claim is submitted with an Assessment Centre group number for any fee code other than H409A or H410A, the claim will reject “ESF-Not eligible to bill FSC.”
- If a claim is submitted for H409A/H410A and billed with any group number other than an Assessment Centre, the claim will reject “ESF-Not eligible to bill FSC”.
- H409A/H410A are excluded non-core services in all Primary Care Patient Enrolment Models and all Primary Care Specialized contracts/agreements.
- H409A/H410A will pay fee-for-service when submitted by any physician who participates in Assessment Centre work.
- If you’re rendering services at the Assessment Centre, you are not required to apply for affiliation to the Group, but are required to submit your claims for rendered services in conjunction with the group number.You should contact your Assessment Centre administrator to obtain their group number in order to submit their claims.
How to Bill H409/H410 (Hourly fee)
Since H409 and H410 are hourly fees, you need to create a claim using a universal patient and submit units as hours. To do this on Dr.Bill, write in to our support team and let us know you’d like to bill H409/H410. We’ll help you set up the correct patient and make sure your settings are correct.
On H409 and H410 claims you need to have the following information:
- the field labeled ‘group number’ you need to add the group number for the assessment centre you worked at (you s
hould be able to get this number from the admin at the centre). - the service date you worked at the assessment center
- for the number of hours you worked, add this in as the number of units.
Temporary Codes Summary
K080: minor assessment of a patient by telephone or video, or advice or information by telephone or video to a patient’s representative regarding health maintenance, diagnosis, treatment and/or prognosis-$23.75
K081: a) intermediate assessment of a patient by telephone or video, or advice or information by telephone or video to a patient’s representative regarding health maintenance, diagnosis, treatment and/or prognosis, if the service lasts a minimum of 10 minutes; or
b) psychotherapy, psychiatric or primary mental health care, counselling or interview conducted by telephone or video, if the service lasts a minimum of 10 minutes-$36.85
K082: psychotherapy, psychiatric or primary mental health care, counselling or interview conducted by telephone or video per unit (unit means half hour or major part thereof) per unit-$67.75
K083: specialist consultation or visit by telephone or video payable in increments of $5.00.
For rules and examples please see New OHIP Fee Codes in response to COVID-19 Pandemic.
Sessional Fee Schedule Code Summary
H409: COVID-19 Sessional Unit per one hour period or major part thereof, Monday to Friday 7 a.m to 5 p.m-$170.00
H410: COVID-19 Sessional Unit per one hour period or major part thereof, Saturdays, Sundays, holidays, or Monday to Friday 5 p.m to 7 a.m-$220.00
New Diagnostic Code for COVID-19
Effective March 14, 2020, a new diagnostic code has been created for the COVID-19 outbreak.
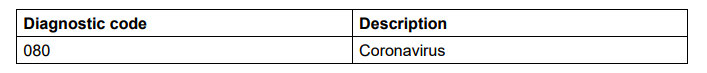
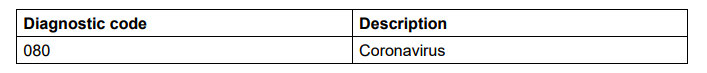
The new diagnostic code should be used when treating patients with suspected or confirmed COVID-19 and/or when treating a patient by telephone/video for suspected or confirmed COVID-19. Use the appropriate diagnostic code when treating a patient for unrelated diagnoses by telephone/video due to COVID-19 related concerns.
If, at any time, you have any questions don’t hesitate to get in touch. Otherwise, please check back to the COVID-19 Resource centre for more updates.
This article offers general information only and is not intended as legal, financial or other professional advice. A professional advisor should be consulted regarding your specific situation. While information presented is believed to be factual and current, its accuracy is not guaranteed and it should not be regarded as a complete analysis of the subjects discussed. All expressions of opinion reflect the judgment of the author(s) as of the date of publication and are subject to change. No endorsement of any third parties or their advice, opinions, information, products or services is expressly given or implied by RBC Ventures Inc. or its affiliates.

Claim Your $150 Credit!
Get a $150 Credit when you sign up for Dr.Bill*. No credit card required.
*Terms and conditions apply.